
Quantitative Reduction of Left Ventricular Summit Extrasystoles through Exit Site Attenuation
 Ablation of ventricular extrasystoles (VES) from the left ventricular summit (LVS) is challenging due to juxtaposed coronary arteries. Ablation at accessible potential exit sites (anterior interventricular vein (AIV), left ventricular outflow tract (LVOT)/aortomitral continuity (AMC), and posterior right ventricular outflow tract (RVOT)) was utilized for potential exit site attenuation and reduction of VES burden.
Ablation of ventricular extrasystoles (VES) from the left ventricular summit (LVS) is challenging due to juxtaposed coronary arteries. Ablation at accessible potential exit sites (anterior interventricular vein (AIV), left ventricular outflow tract (LVOT)/aortomitral continuity (AMC), and posterior right ventricular outflow tract (RVOT)) was utilized for potential exit site attenuation and reduction of VES burden.
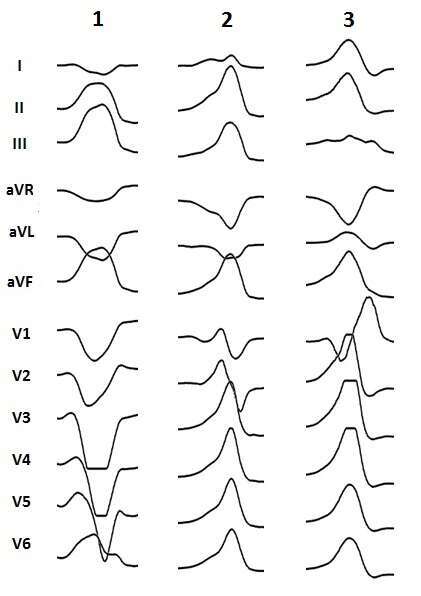
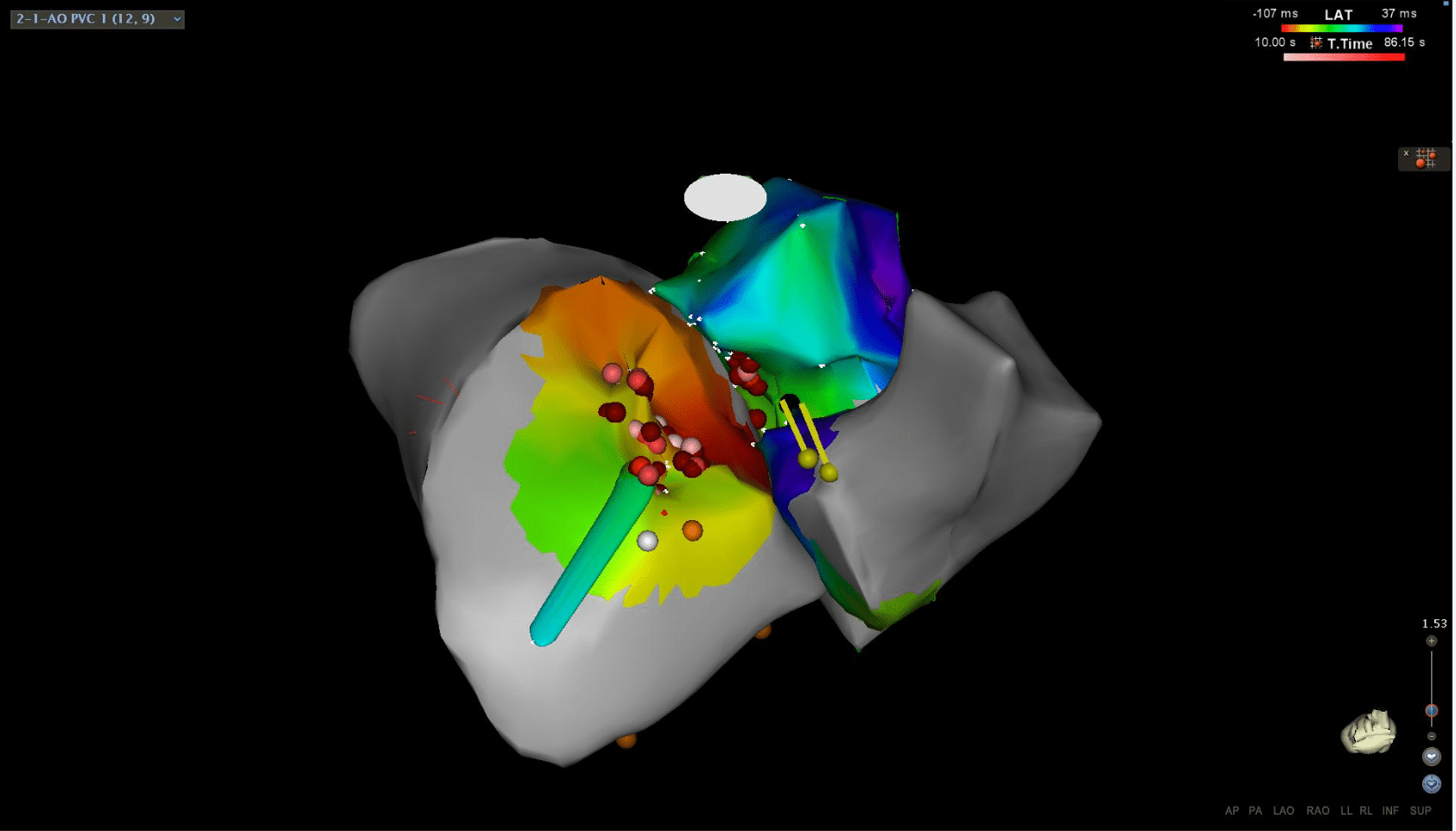
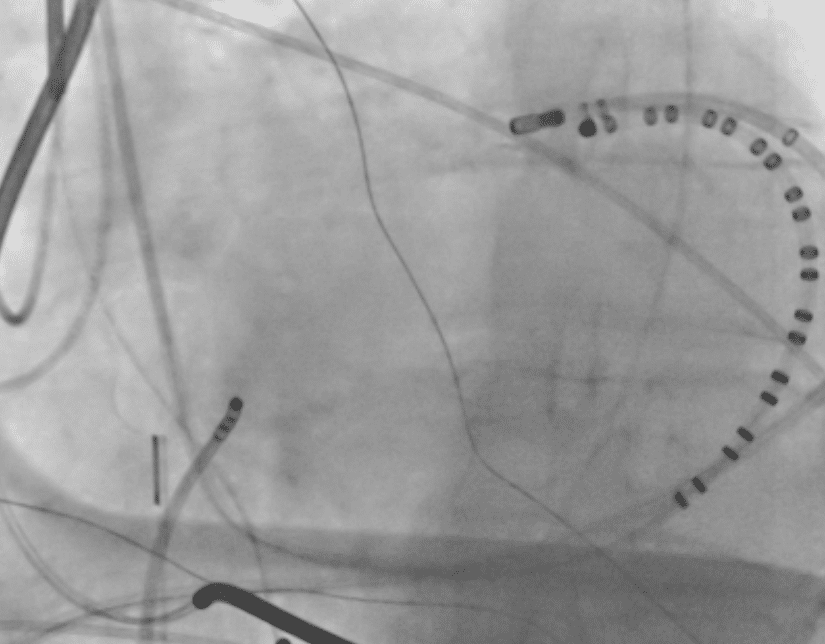
Case 1: A 57 y/o female with recurrent VES induced ventricular fibrillation, ICD shocks and prior failed ablation of VES in the RVOT. A repeat procedure identified the VES with earliest local electrograms (20 ms pre-QRS) at both the posterior RVOT and anterior LVOT. Ablation at these sites resulted incomplete suppression of the VES. There have been no ICD shocks in 6 weeks.
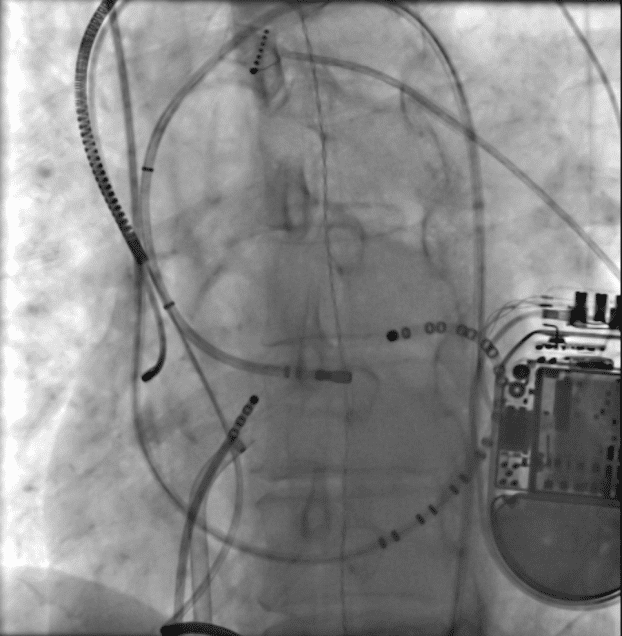
Case 2: A 68 y/o female with symptomatic ventricular bigeminy and prior failed ablation subsequently developed cardiomyopathy (EF 40%) , complete heart block treated with CRT-P and suboptimal resynchronization underwent repeat ablation of her clinical VES. The earliest local activation was at the posterior RVOT (26ms pre-QRS) and aortomitral continuity (28ms pre-QRS). Ablation at these sites resulted in markedly reduced VES frequency. The LVEF is 64% and biventricular pacing is >90% at 2 months followup versus 75% pre-ablation.
Case 3: A 63 y/o male with hemochromatosis and recurrent ventricular tachycardia & ICD shocks after three prior unsuccessful ablation attempts underwent a repeat procedure where the earliest local activation was 31 msec pre-QRS at the anterior AMC and 10 msec pre-QRS at the AIV for the clinical VES. Ablation at all these areas resulted in complete suppression of VES. No ICD shocks have occurred at 4 weeks follow-up
The proximity of the left main coronary artery and LVS makes ablation challenging in this area. Success has been demonstrated with open sternotomy and direct visualization for ablation although this can be associated with significant morbidity. An alternative, such as exit site attenuation may produce significant clinical improvement.

Powered by Eventact EMS