
Brugada’s Algorithm Demonstrates Superior Accuracy and Interobserver Agreement Over aVR Vereckei’s Algorithm When Applied by Non-Cardiologists
2Internal Medicine, Mayo Clinic Minnesota
Aims: The electrocardiograpm (ECG) remains the most widely available non-invasive test to rapidly diagnose ventricular tachycardia (VT) and wide-complex supraventricular tachycardia (SVT). The Vereckei aVR and Brugada algorithms have emerged as the most recognized and frequently used ECG algorithms to differentiate VT and wide-complex SVT among non-cardiologist (NC) providers. Our purpose was to evaluate individual algorithm’s accuracy and interobserver agreement when applied by NCs on unselected ECGs with a confirmed clinical diagnosis.
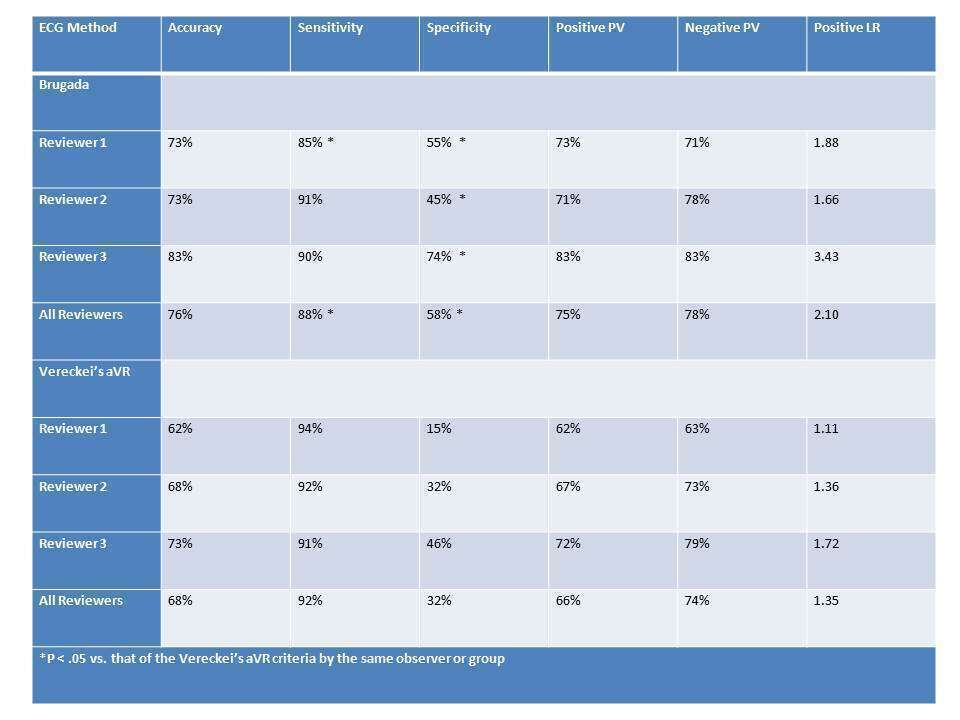
Methods and Results: Three internal medicine residents interpreted a collection of 12-lead ECGs in two separate blinded interpretation sessions using the Vereckei aVR and Brugada algorithms. Each interpreter was provided algorithm instruction and reference materials to assist in ECG interpretation. Each ECG required clinical confirmation of VT or SVT by the patient’s overseeing attending cardiologist. Each study participant interpreted 273 ECGs (162 VT, 111 SVT) from 190 patients for a total of 819 discrete interpretation events per session. Both algorithms demonstrated high sensitivity but inferior specificity for diagnosing VT. Overall (Table), Brugada’s method showed higher accuracy (75% positive predictive value, 2.1 positive likelihood ratio) than the Vereckei aVR algorithm (66% positive predictive value, 1.35 positive likelihood ratio). Accuracy increased for both algorithms as a function of number of ECG’s interpreted (Fig 1 and 2). Interobserver agreement was fair when using Brugada’s (kappa 0.23-0.48) and poor for Vereckei’s method (kappa -0.09-0.38).
Conclusions: despite being more time-consuming, Brugada’s algorithm showed superior accuracy and interobserver agreement for discrimination of wide-complex tachycardias when applied by non-cardiologists. The significantly lower accuracy of these algorithms in “real-life” as compared to original reports suggests the ongoing need for improved diagnostic methods for non-cardiologists to differentiate wide-complex tachycardias.
Powered by Eventact EMS