
Cardiac Resynchronization Therapy with Pacing (CRT-P) versus with Defibrillation (CRT-D) in Octogenarian Patients with Heart Failure in a Real-World Setting
2The Israeli Association for Cardiovascular Trials, Leviev Heart Center, Sheba Medical Center, Tel Hashomer
3Department of Cardiology, Rambam Medical Center, Haifa
Background: Recent studies showed that in patients with LBBB and HF symptoms, aging is associated with a significant decrease in the incidence of ventricular tachy-arrhythmias and of appropriate ICD shocks. These findings suggest that CRT-P may confer similar benefit to CRT-D in older patients. We compared the effectiveness of CRT-P versus CRT-D in octogenarian patients with HF.
Methods: We compared consecutive patients aged ≥80y that underwent CRT-P implantation in Barzilai MC between 2006-2013 (n=142) to a control group aged ≥80y that were implanted with CRT-D for primary prevention indication and were enrolled in the Israeli ICD Registry between 7/2010- 2/2015 (n=104).
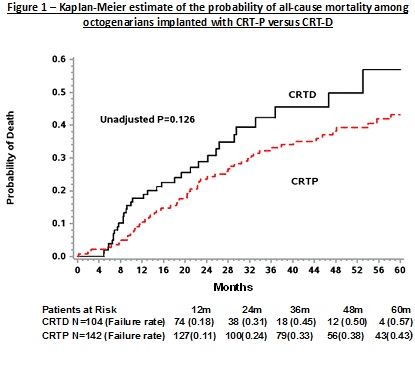
Results: Among the total 246 study patients, mean age was 83.5±3 years. 74% were males and 66% had IHD. Kaplan-Meier survival analysis showed that at 5 years of follow-up the cumulative probability of all-cause mortality was 43% in the CRT-P group as compared with 57% in the CRT-D group (log-rank p=0.126 for the overall difference during follow-up between the two groups; Figure). Consistently, the adjusted Hazard Ratio (HR) of mortality between the two groups (adjusted for age, sex and propensity score) was 1.27 (95% CI 0.74-2.16, p=0.37). Kaplan-Meier analysis also showed no statistical difference for the combination of death and first HF hospitalization between the two groups (p=0.359) and the adjusted HR was 1.17 (95% CI 0.69-1.97, p=0.55). A cox proportional hazard with competing risk model showed that re-hospitalizations for cardiac cause were not different for the two groups (adjusted HR 1.35, 95% CI 0.7-2.6, p=0.37).
Conclusion: In a real-world scenario, CRT-P is not significantly different from CRT-D regarding rate of mortality and the combination of HF and mortality in octogenarians with low ejection fraction and HF. These findings suggest that, in older patients, implantation of CRT-P alone without defibrillator therapy may be considered as an alternative to CRT-D.
Powered by Eventact EMS