
Impact of the Presence and Treatment Status of Diabetes on Long-term Mortality Following Coronary Angiography
Background: Diabetes mellitus confers increased risk for coronary artery disease (CAD) and mortality. We aimed to determine the impact of diabetes and its treatment, on long-term mortality following coronary angiography for evaluation or therapy of CAD.
Methods: Retrospective analysis was performed of 14,337 consecutive patients, undergoing coronary angiography for stable or acute coronary syndromes (ACS) between the years 2000 and 06/2015. Patient characteristics and long-term mortality were evaluated by Cox regression analysis according to diabetes status (no-diabetes versus diet only, oral-hypoglycemics or insulin treated diabetes) and indication for coronary angiography.
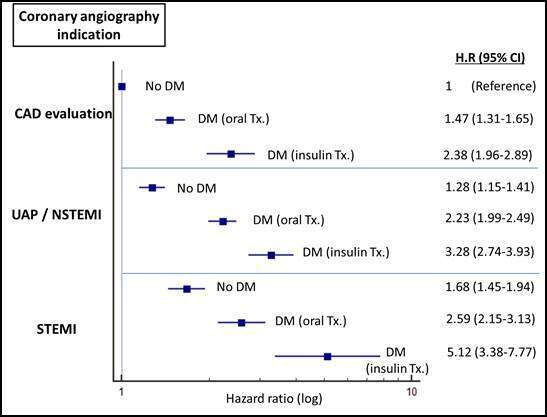
Results: Diabetes was documented in 5,279 (37%) patients, of whom 304 were treated by diet only, 4,002 with oral hypoglycemics and 973 by insulin. The presence and treatment status of diabetes was associated with hypertension, hyperlipidemia, renal failure, higher BMI and female gender, as well as previous percutaneous coronary interventions. In comparison to lack of diabetes (reference), the adjusted hazard ratio (HR) for long-term mortality during a median follow-up period of 78 months (IQR 40-119) for diet only diabetes was 1.41 (95% C.I, 1.11-1.80), p=0.006, for oral hypoglycemic treated 1.63 (1.51-1.77), p<0.001, and for insulin treated diabetes 2.50 (2.20-2.85), p(Figure) and remained significant after further adjustment for cardiac catheterization indication. Diabetes was a stronger predictor of long-term mortality than ACS so that the relative risk for mortality was higher in medically treated diabetics without ACS, compared to ACS patients without diabetes (HR 1.21, 95% C.I 1.08-1.35, p=0.001).
Conclusions: In patients referred for coronary angiography diabetes was an independent predictor of long-term mortality, regardless of the clinical syndrome, and mortality was directly related to treatment status/intensity.
Powered by Eventact EMS