
Impact of Renal Dysfunction on Transcatheter Aortic Valve Replacement Outcome in a Large Multicenter Cohort
2Cardiology, Ferrarotto Hospital
3Cardiology, Inselspital University Hospital, Bern
4Cardiology, Keio University Hospital
5Cardiology, Institute Cardiovasculaire Paris Sud
6Cardiology, Galway University Hospital
7Cardiology Department, CHRU, Lille
8Cardiology, University Hospital, Antwerp
9Cardiology, Sheba Medical Center, Ramat Gan
10Cardiology, Bonn University Hospital
Background: Patients with advanced chronic renal dysfunction were excluded from randomized Transcatheter Aortic Valve Replacement trials. The potential impact of chronic renal disease on TAVR prognosis is not fully understood.
Objectives: We sought to evaluate outcomes within a large cohort of patients undergoing TAVR distinguished by renal function.
Methods: Baseline characteristics, procedural data and follow-up findings were collected from 10 high-volume centers in Europe, Israel and Japan among TAVR treated patients with and without renal disease.
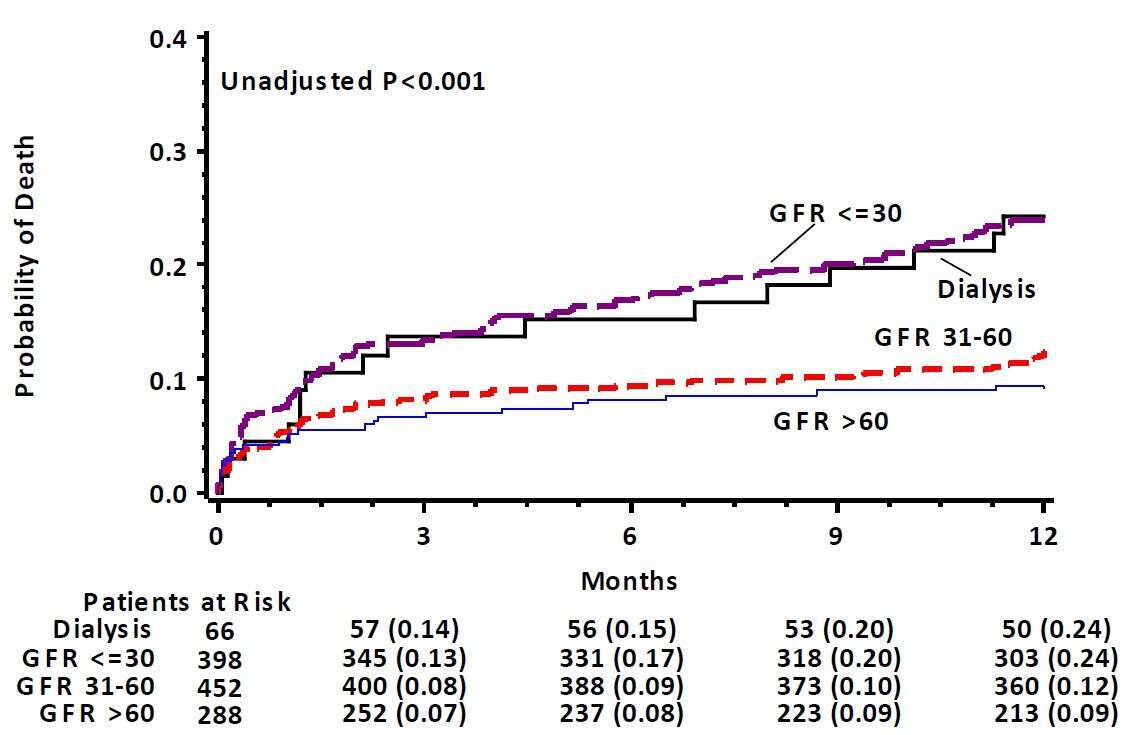
Results: Patients (n=1204) were divided into 4 groups according to pre-TAVR glomerular filtration rate (eGFR): group I (eGFR ≥60) n=288 (female 44.8%), group II (eGFR ≥30 <60) n=452 (female 61.1%), group III (eGFR <30) n=398 (female 61.1%) and group IV (on dialysis) n=66 (female 31.3%). Mean age was 78.5±7, 82.3±5, 83.8±5and 76.1±7 y/o for patients in group I, II, III and IV; respectively (p<0.001). Mean Society of Thoracic Surgeons (STS) score was higher in patients with lower pre-procedural eGFR: 5.4 (3.7-7.1) in group I, 6.0 (4.3-9) in group II, 8.8 (6.0-12.6) in group III and 10.1 (7.7-16) in group IV; (p <0.001).
Rates of all-cause mortality at 1-year follow up were higher for patients with lower pre-procedural eGFR (Figure) By multivariate analysis, every 10-mg/dL decrease in eGFR were associated with a respective 19% (p<0.001), 14% (p=0.018), 35% (p<0.001), and 16% (p=0.007) increase in the risk of death, cardiovascular death, major bleeding, and valve failure, respectively. eGFR did not affect the risk for CVA or pacemaker implantation.
Conclusions: Among patients undergoing TAVR, baseline renal dysfunction is an important independent predictor for all-cause mortality with incremental prognostic impact.
Powered by Eventact EMS