
Treatment Gaps in Management of Patients Following Acute Myocardial Infarction: Analysis of Real-World Data
2Sackler Faculty of Medicine, Tel-Aviv University, Tel Aviv
3Global Health Outcomes, C.O.R.E., Merck & Company, Inc., Rahway, NJ
4Medical Affairs, MSD Israel, Hod Hasharon
5Internal department E, Tel Aviv Sourasky Medical Center, Tel Aviv
Cardiovascular diseases are the leading causes of death and myocardial infarction (MI) accounts for nearly half of cardiovascular-related deaths.
We characterize long-term management of patients who experienced an MI between 01/2009 and 12/2010 among adult members Maccabi Healthcare Services, using linked, longitudinal electronic medical records. Patients with a history of CVA or TIA were excluded from the study to focus on those whose antiplatelet treatment wouldn’t substantially be influenced by bleeding risk.
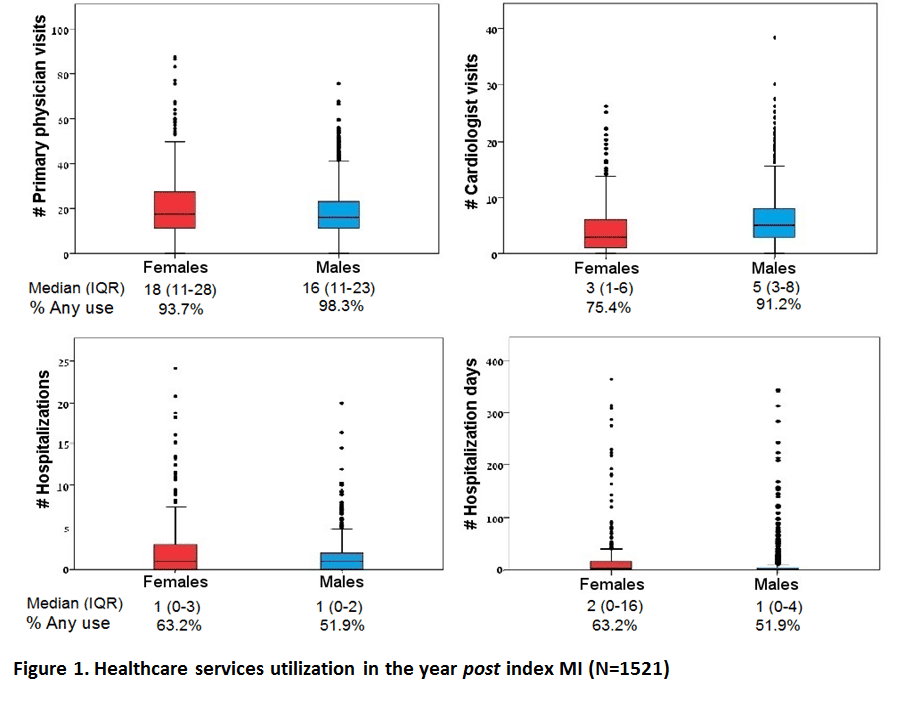
We identified 1649 eligible incident MI patients (75% men, mean age=64.7±14.2 y). Of 1521 patients surviving at least 60 days from hospital discharge, men were on average 12 years younger than women (60.6 y vs. 72.5 y, respectively) and with less comorbidity at index MI. More women than men remained untreated at 60 days post hospital discharge (13.2% vs. 3.2%, respectively, p<0.001) and were not seen by a cardiologist during the following year (25% vs. 9%, respectively, p<0.001). Among 1425 patients eligible for treatment analysis, women were less likely to be treated with dual antiplatelet therapy (DAPT, clopidogrel + acetylsalicylic acid (ASA)) than men (70% vs. 52%, respectively, p<0.001).
The study results indicate that a considerable proportion of post-MI patients go untreated with antiplatelet therapy and without seeing a cardiologist, particularly among women. Further efforts are required to assess how gender may drive disease management and subsequently prognosis among patients experiencing an MI.
Powered by Eventact EMS