
The Impact of Gender Mismatching on Early and Late Outcomes Following Heart Transplantation
2Cardiothoracic Surgery, Sheba Medical Center
Introduction: The role of donor/recipient gender matching on the long–term rejection process and clinical outcomes following heart transplantation (HT) is still controversial. We aim to investigate the impact of gender matching on early and long term outcomes following HT.
Methods: The study population comprised 166 patients who underwent HT between 1991 and 2013 and were prospectively followed up in a tertiary referral center. Early and late
outcomes were assessed by the type of donor-recipient gender match (primary
Analysis: female donor-male recipient [FD-MR, n=36] vs. male donor-male recipient
[MD-MR, n=109]).
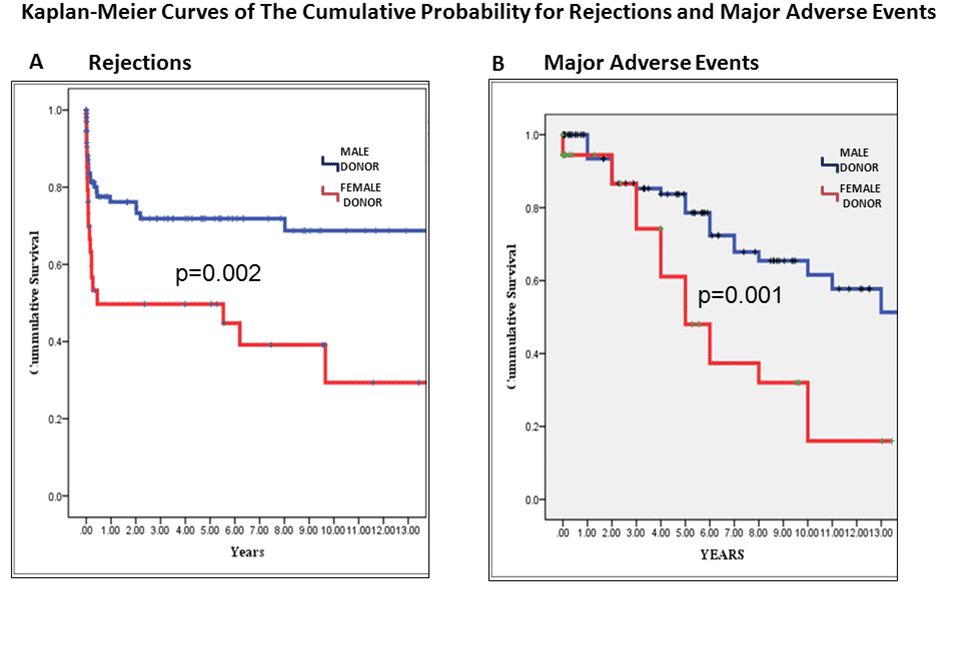
Results: The FD-MR group experienced significantly higher rates of early major rejections per patient as compared with the MD-MR group (1.2±1.6 vs. 0.4±0.8; p=0.001), higher rates of overall major rejections (16 vs. 5.5 per 100 person years; p< 0.05) and higher rate of cardiac allograft vasculopathy (43% vs. 20%; p=0.01). Multivariate analysis showed that FD-MR status was associated with >2.5-fold (p=0.03) increase in the risk for rejections and with a >3-fold (p=0.01) increase in the risk for major adverse events during follow-up. Kaplan-Meier survival analysis showed that the cumulative probabilities of survival free of rejections and major adverse events were significantly higher in MD-MR group (p=0.002 and 0.001 respectively [Figure]). Risk of death by donor-recipient gender match did not differ between groups. Early mortality, need for inotropic support, length of hospital stay and major perioperative adverse events did not differ between the FD-MR and MD-MR groups.
Conclusions: Donor-recipient gender mismatch is a powerful independent predictor of early and late rejections and long-term major adverse events following heart transplantation.
Powered by Eventact EMS