
Trends of Early and Late Rejection Rates Following Heart Transplantation Over the Past Two Decades: Real world Data from a National Tertiary Center Registry
2Cardiothoracic Surgery, Sheba Medical Center
3The Israeli Association for Cardiovascular Trials, Sheba Medical Center
Introduction: Over the past two decades there have been major changes in the management of heart transplant (HT) patients. We aimed to evaluate how these changes affected early, intermediate, and late rejection rates.
Methods: Data on 240 patients who underwent HT between 1991-2015, and prospectively followed-up was analyzed . A total of 2458 biopsies were performed. Rejections were categorized as major (cellular grade 2R, 3R and humoral AMR1 according to the 2004 revised classification) vs. minor or none. P-value for trend was used to assess the statistical significance of changes in the rates of early (0-3 months), intermediate (>3-12 months), and late (>12 months) rejection. All patients were treated with triple-drug immunosuppression regimen (cyclosporine 1991-2006 or tacrolimus 2006-2015 , azathioprine 1991-1996 or mycophenolate mofetil 1996-2015, and corticosteroids. Since 2009, a minority of patients received everolimus. Also, all patients received induction therapy with anti-thymocyte globulin.
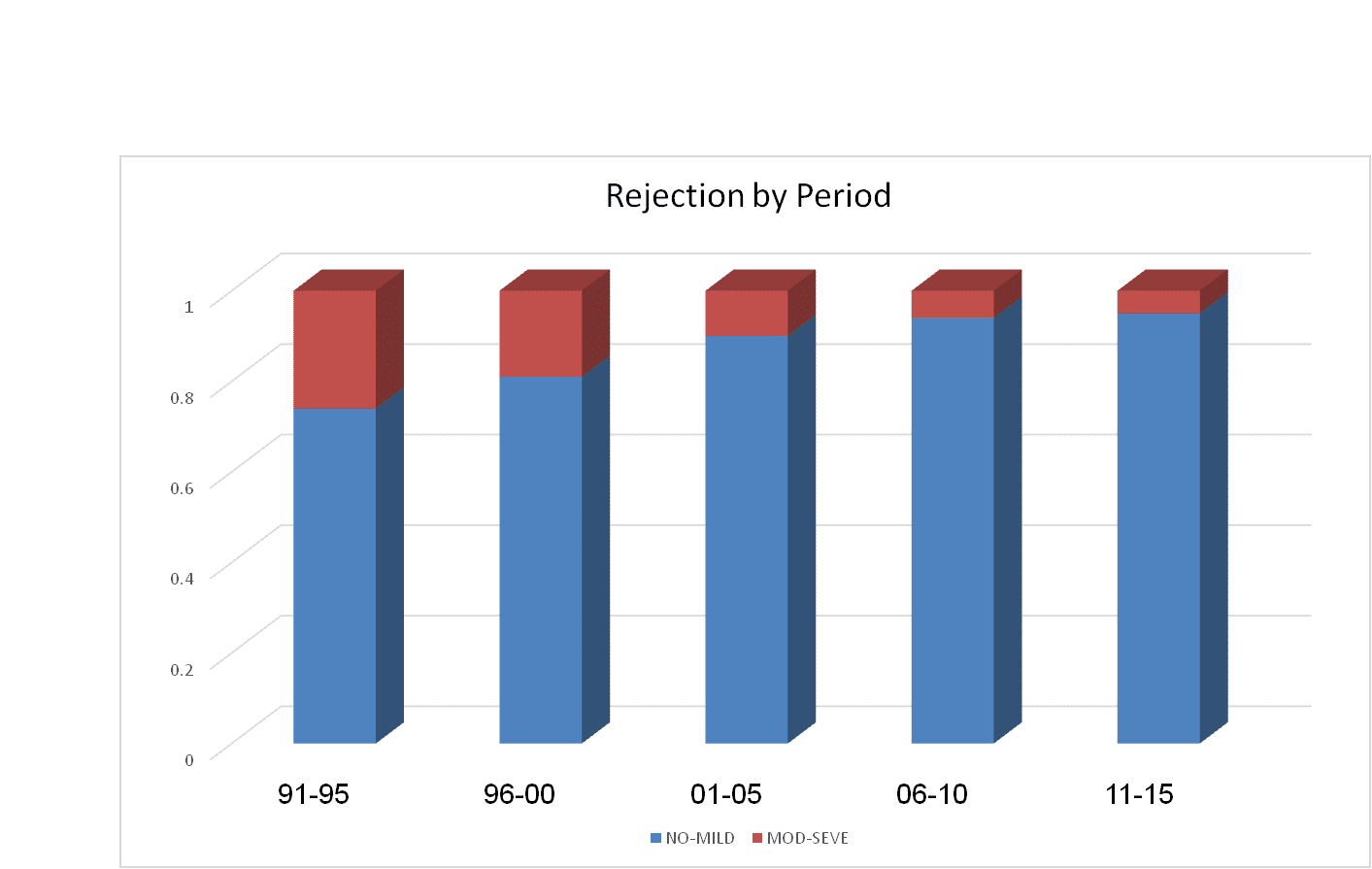
Results: Total risk for major rejection was significantly higher at early eras: 26% during 1991-1995, 19% at 1996-2000, 10% during 2001-2005 6% at 2006-2010 and 5% during 2010-2015 (p-value for trend < 0.001 [Figure]). Consistent with those findings, multivariate logistic regression modeling that the risk for major rejection was >3-fold higher between the years 1991-2005 as compared to 2006-2015 (OR = 3.30 [95% CI 2.02 – 5.38] p<0.001). Furthermore, the significant reduction in major rejection rates over this time period was consistent when the rates of early, intermediate, and late rejections were assessed separately (p-value for trend < 0.001 for all), with the most prominent decline shown in the rates of late rejection from 80% between the years 1991-1995 to <1% after 2011.
Conclusions: Major rejection rates following HT have significantly declined over the past two decades, with consistent declines in early, intermediate, and late rejection rates. These data may trigger reevaluation of immunosuppression protocols.
Powered by Eventact EMS