
Factors Associated with Adverse Outcomes in Ambulatory Heart Failure Patients
2Cardiology Department, Shaare Tzedek Medical Center, Jerusalem
3Cardiology Department, Rabin Medical Center, affiliated to the Sacker Faculty of Medicine, Tel Aviv University, Petah Tikva
Background: Heart failure (HF) is a deadly condition in which community studies demonstrate 1-year mortality of 30-40% and 5-year mortality of 60-70%. However, individual patient prognostication remains a challenge, due in part to the changing landscape of HF management over past decades.
Objectives: Identifying factors associated with poor prognosis in HF patients treated at a tertiary clinic.
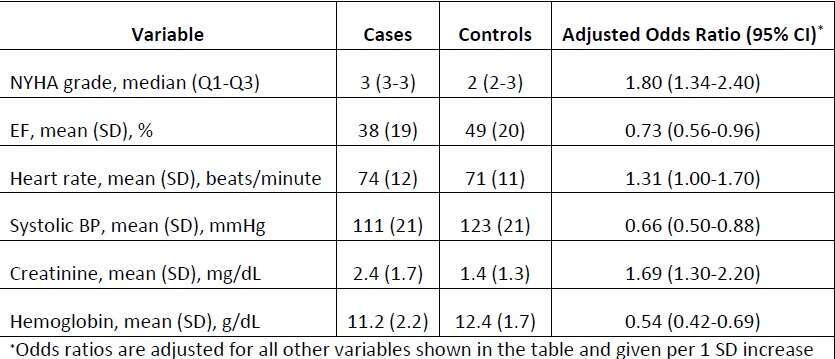
Methods: Using electronic data from various sources, a case-control study was conducted among HF patients treated at Rabin tertiary HF clinic during 2008-2013. Case patients (n=184, all cases that occurred during the study period) were defined using a composite outcome of death (n=150), LVAD implant (n=25) and heart transplant (n=9). Sociodemographic, clinical, physical, echocardiographic, and laboratory variables were compared between cases and 287 unmatched control subjects, free of the composite outcome at the index date. Patients’ last recorded data were used. Together, these comprise the entire patient population of the clinic for the study period. A logistic regression model was constructed to identify factors associated with the outcome.
Results: For the entire study population, mean (SD) patient age was 65 (12) years and 80% were males. NYHA class ≥3 was present in 45% of patients, whereas ejection fraction (EF) ≤40% was found in 43%. While neither age nor gender was associated with the outcome, various factors showed considerable prognostic value, among them NYHA class, hemoglobin and creatinine levels (Table).
Conclusion: The results validate known risk factors such as NYHA class and reduced EF and provoke other variables such as heart rate, systolic pressure, creatinine levels and hemoglobin as possible prognostic markers in HF.
Powered by Eventact EMS