
Decreased Admission Albumin Level is an Independent Predictor of Long-term (10-years) Mortality Following Acute Myocardial Infarction
2Cardiology, Soroka University Medical Center, faculty of Health Sciences, Ben-Gurion University of the Negev, Beer Sheva
3Unit of Nursing Research, Soroka University Medical Center, Faculty of Health Sciences, Ben-Gurion University of the Negev, Beer Sheva
Background: Decreased Serum albumin level (SAL) was reported to be associated with increased risk of cardiovascular events and short term-mortality in patients with acute myocardial infarction (AMI)
Objectives: To evaluate the post AMI long term (up-to 10-years) prognostic value of admission SAL.
Methods: Patients who had been admitted in a tertiary medical center for AMI 2002 through 20012 and discharged alive were studied. Exclusion criteria were: active infections, inflammatory diseases, advanced renal (Creatinine>3 mg/dl) or liver (Bilirubin>5 mg/dl) failure, malignancy, severe congestive heart failure (Ejection fraction<20%), severe valvular disease, missing SAL during hospitalization. The SALs were categorized as following: <3.4, 3.4-3.7, 3.7-3.9, 3.9-4.1and >4.1 mg/dl. The primary outcome was all-cause mortality for up to 10-years post AMI.
Results: overall 8,750 out of 12,535 patients were included. Patients with reduced albumin levels were older, higher rate of women, had congestive heart failure, chronic renal failure, diabetes mellitus and STEMI, 3 vessel disease, and in-hospital complications. while the prevalence of chronic ischemic coronary disease, dyslipidemia, smokers, obesity and family history of ischemic heart disease, was lower. Mortality rates throughout the follow-up period increased as albumin levels decreased with 17.6%, 24%, 28.5%, 38.6%, 57.5% for SAL of >4.1, 3.9-4.1, 3.7-3.9, 3.4-3.7, <3.4, respectively, (P<0.001). Unadjusted and adjusted hazard ratio for mortality increased significantly as SAL were lower (figure 1). Decreased SAL was found to be a strong independent predictor of long-term mortality in a multivariate model.
Conclusions: Decreased SAL on admission, including levels within "normal" clinical range, is an independent predictor for long-term all-cause mortality in hospital survivors of AMI. Further evaluation of the pathophysiological mechanisms and potential interventions to increase SAL following AMI are warranted.
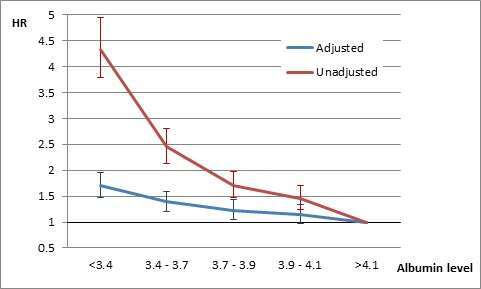
Figure 1. Unadjusted and adjusted relative risk for long-term all-cause mortality by the category of serum albumin level
Powered by Eventact EMS