
Using Multidisciplinary Approach Pulmonary Thromboendarterectomy is Safe with Excellent Late Outcomes
2Pulmonology, Sheba Medical Center, Tel Hashomer, affiliated with the Sackler School of Medicine, Tel Aviv University, Tel Aviv
3Anaesthesiology, Sheba Medical Center, Tel Hashomer, affiliated with the Sackler School of Medicine, Tel Aviv University, Tel Aviv
4Cardiothoracic Surgery, Universitatsklinikum des Saarlandes, Homburg
Introduction: Pulmonary thromboendarterectomy (PEA) Surgery is the preferred definitive treatment for chronic thromboembolic pulmonary hypertension (CTEPH). Pre and post-operative evaluation and treatment are complex and require multi-team approach; pulmonologists, anesthesia, intensive care specialists and specifically trained cardiac surgery team. . Coronary angiography and right heart catheterization and pulmonary angiography are routinely performed prior to surgery. Pulmonary thromboendarterectomy necessitate open-heart surgery with periods of deep hypothermic circulatory arrest. Hemodynamic improvement is anticipated following thromboendarterectomy, with marked reductions in pulmonary artery pressures and pulmonary vascular resistance. Outcomes continue to improve in recent decades. Objective – to evaluate the safety of the operation as well as the objective and subjective improvement as reflected with mean PAP and clinical improvement respectively
Methods: since 2007 21 patients with CTEPH underwent PEA in our institution; all patients had severe right side heart failure, with mean functional capacity (FC) of 2.94±0.63, severe PAP, and reduced RV function.
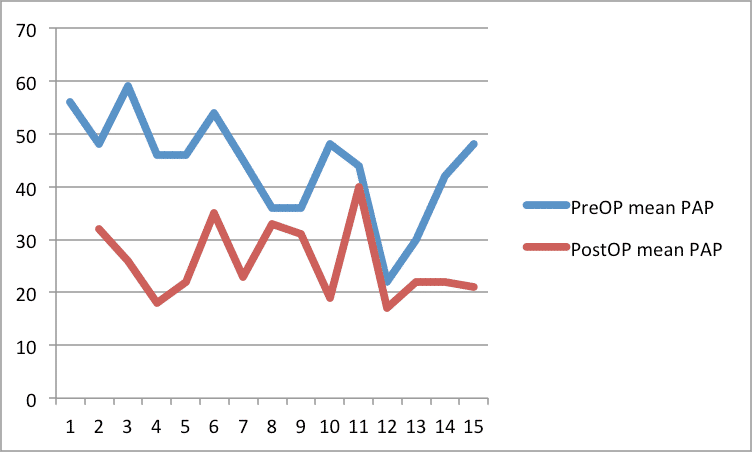
Results: there was one operative death, mean PAP was significantly reduced compared to pre-operative mean PAP (43 mmHg vs 26 mmHg p<0.001, Fig 1). cardiac output, was also significantly higher after PEA (3.7 L/min vs 5.7 L/min, p<0.002). FU was 32 months (±29, ranged 2-102 months); there was no late mortality. Mean FC improved from 2.94±0.63 to 1.7±0.94.
Conclusion: PEA is a safe, short term benefits of the procedure are evident in the significant improvement in Cardiac output and lower mean PAP.
Powered by Eventact EMS