
Neonatal Alloimmune Thrombocytopenia: A Retrospective Analysis of Clinical and Laboratory Findings in Slovenian Patients
2Department of Perinatology, University Medical Centre Maribor, Division of Gynecology and Perinatology
3Department of Gynecology and Obstretics, University Medical Centre Ljubljana, Division of Perinatology
4Platelet Immunology Laboratory, Blood Transfusion Centre of Slovenia
Background: Neonatal alloimmune thrombocytopenia (NAIT) results from transplacental transmission and binding of alloimmune antibodies on child`s platelets (PLT) antigens. It is a rare disease with unpredictable course.
Objectives: To evaluate the incidence, aetiology, clinical course and adherence of recommendations for treatment of NAIT in Slovenia.
Methods: Medical documentation of newborns with NAIT born in Slovenia between 1996 and 2016 was studied. Cases were identified from the Slovenian Blood transfusion centre database. NAIT inclusion criteria were neonatal thrombocytopenia and the presence of PLT antibodies (PLT-Ab) in mother and/or newborn.
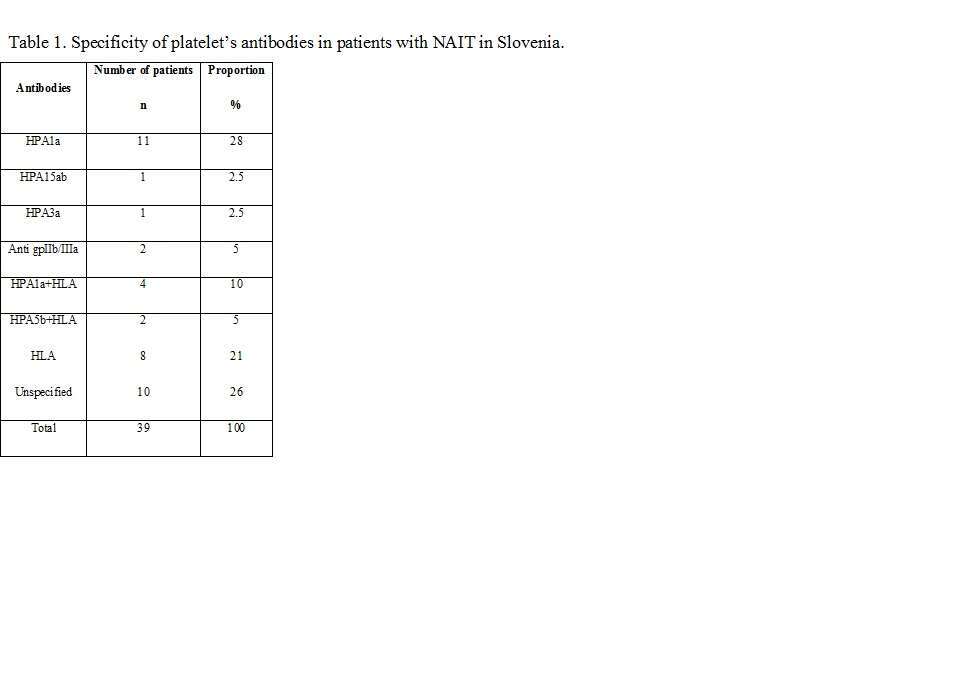
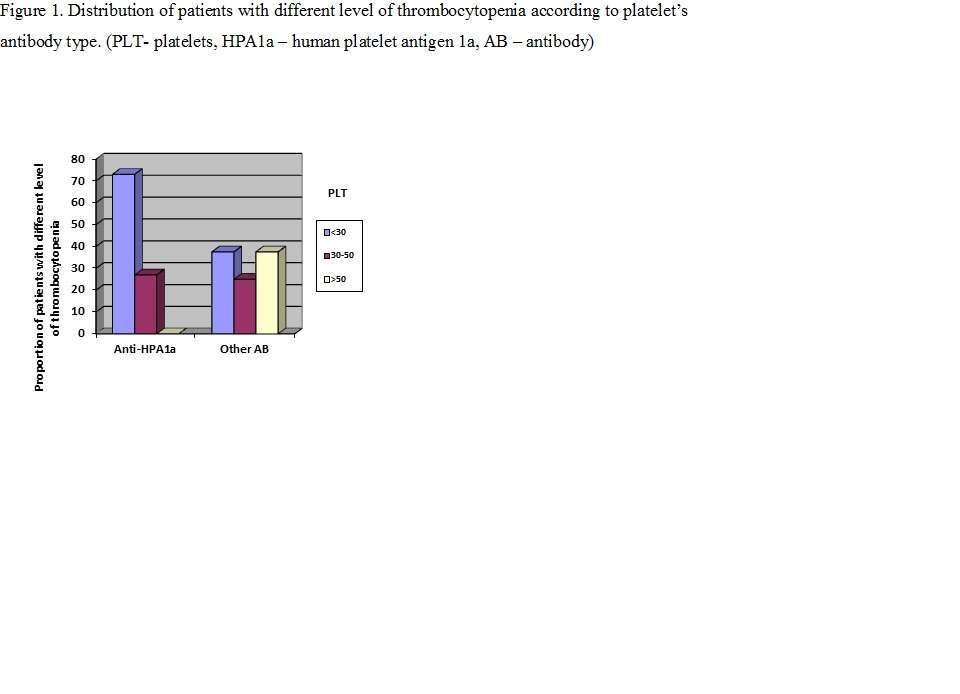
Results: PLT-Ab were detected in 65 out of 229 referrals (due to neonatal thrombocytopenia, recurrent miscarriage or intrauterine fetal death). 16 medical records of the newborns were not available. 37 from the remaining 49 with PLT-Ab developed thrombocytopenia (incidence 0.1/1000 live births). Specificity of PLT-Ab in Slovenian patients is shown in Table 1. 15 (38%) of the newborns were anti-HPA-1a positive and 8 (21%) were HLA antibodies positive only. Five mothers needed IVIG prenatally. Two out of 6 mothers with the history of NAIT delivered with C-section. 27 newborns presented with petechiae and/or suffusions and one with intraventricular haemorrhage. Among 9 asymptomatic newborns, 2 had anti-HPA-1a. PLT were lower in newborns with anti-HPA-1a with the lowest value presented earlier (2nd day vs 3rd/4th day) than in the other groups (Figure 1). 8 (20,5%) newborns needed PLT transfusion (PLT-trans), 4 (10%) PLT-trans and IVIG, 1(2,5%) IVIG, and 1(2,5%) PLT-trans, IVIG and steroids.
Conclusion: The most common aetiology of NAIT was anti-HPA-1a but its frequency was lower than reported in the literature. HLA antibodies were frequently identified as the only antibodies in patients with symptomatic thrombocytopenia. Anti-HPA-1a caused more severe thrombocytopenia than other PLT-Ab. Only 35% of newborns with PLT <30x109/L received therapy and C-section was not performed in all cases with history of NAIT.

Powered by Eventact EMS