
Outcomes in East London Premature Babies on Home Oxygen: Growth and Readmissions
Background: Preterm infants with bronchopulmonary dysplasia are a vulnerable group of babies. Home oxygen has the advantage of early discharge to allow family life normalisation, hopefully facilitating growth. We carried out a study to evaluate the growth and readmission rates.
Method: Data was collected retrospectively with electronic patient records for infants born at the Royal London Hospital between 2011-2014, discharged on home oxygen and followed up in clinic until 2 years old. Growth parameteric SD scores (SDS) were calculated using LMS calculator for Microsoft Excel and data was analysed with non-parametric tests due to the non-normal distribution of the data from small sample size.
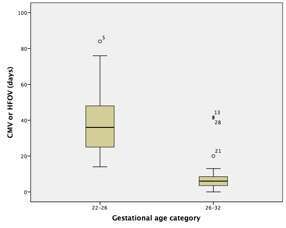
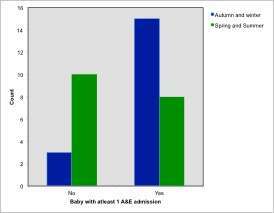
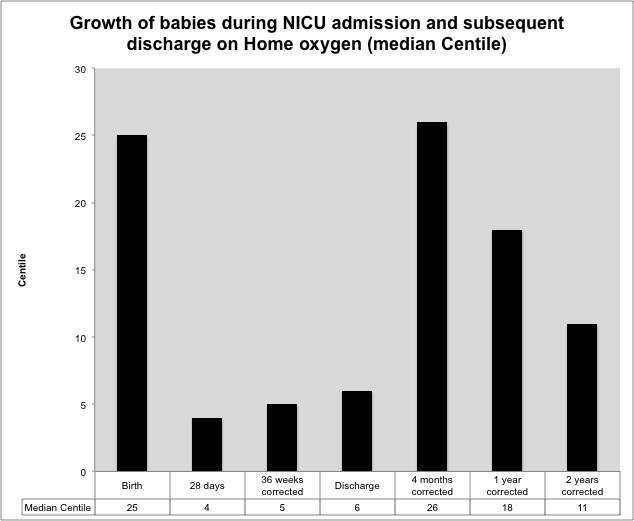
Results: Thirty-six babies met our criteria, born between 22+6 and 30 weeks gestation. Babies less than 26 weeks spent longer on the ventilator (median=36 days) compared to babies born at 26 weeks or more (median 6 days, p<0.001). Already small at birth (median SDS-0.68, 25thcentile), growth is poor during the first 28 days on NICU (median SDS-1.74, 4thcentile) then remains steady at discharge (6thcentile, median SDS-1.53). Following discharge, half of the babies required at least 1 Accident and Emergency attendance within the first year, particularly if discharged over autumn or winter (p<0.015). Half of the episodes resulted in admissions but very few required intensive care (n=4). Growth improved rapidly after discharge, catching up to their birth centile at 4 months corrected (median SDS-0.63, 26th centile). By 1 year corrected, growth velocity tailed off (median SDS-0.93, 18thcentile), although still above the discharge centile.
Conclusion: Growth fell dramatically within the first month, which may reflect their unstable health. Home oxygen leading to normalisation of family life may contribute to rapid growth in the first few months but may also contribute to increased anxiety resulting to unnecessary A&E visits. Improved community support may reduce the burden on acute services.


Powered by Eventact EMS