
Vitamin D Deficiency in Patients with Irritable Bowel Syndrome: Association with Clinical Symptoms, Quality of Life and Inflammatory Cytokines
2Department of Pharmacology and Toxicology, Faculty of Pharmacy, Lorestan University of Medical Sciences
Background: Vitamin D deficiency (VDD) is highly prevalent in gastrointestinal (GI) disorders and might play an important role in the development of these disorders.
Objective: We assessed VDD and also the possible correlation of the serum vitamin D with clinical symptoms, quality of life (QoL) and inflammatory cytokines in IBS patients.
Methods: A total of 90 IBS patients diagnosed according to Rome III criteria (all subtypes) were recruited from the tertiary referral Hospital of the University. Also 90 sex and age matched HCs without GI symptoms took part in the study. Blood was drawn for measurement of the serum 25(OH)D3 levels and cytokines interleukin (IL)-10, IL-17 and tumor necrosis factor (TNF) α. Furthermore, IBS symptoms severity score (IBSSS), IBS quality of life (IBS-QOL) and the severity of GI symptoms were evaluated.
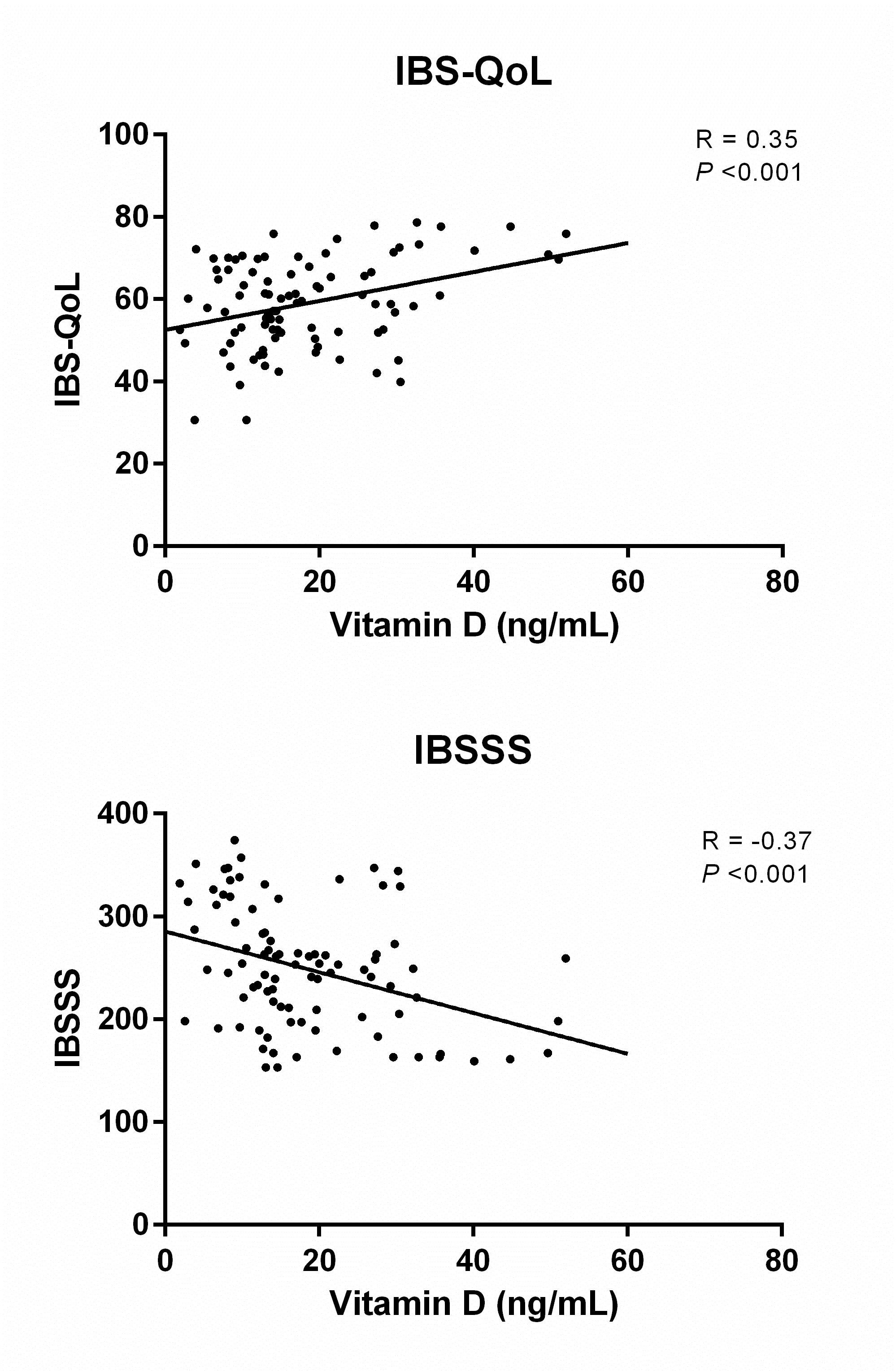
Results: The serum 25(OH)D3 was significantly (P <0.05) lower in IBS patients. When comparing different bowel habit subtypes with HCs, the serum 25(OH)D3 was significantly (P <0.05) lower in diarrhea-predominant IBS (IBS-D). Furthermore, the lower serum 25(OH)D3 was significantly (P <0.05) associated with higher pro-inflammatory cytokines (TNFα and IL-17) and lower anti-inflammatory cytokines (IL-10). The lower serum 25(OH)D3 was significantly (P <0.05) associated with higher severity of GI symptoms and IBSSS, whereas a significant positive association was found between the lower serum 25(OH)D3 and IBS-QoL.
Conclusions: Our study revealed that VDD is highly prevalent in patients with IBS; especially, in IBS-D. VDD is correlated with the higher severity of the IBS symptoms and lower QoL.

Powered by Eventact EMS