
Impact of Evidence-Based Behavior Change Communication on Infant and Young Child Feeding (IYCF) Practices in Tribal Gujarat, India
2Central Research Services, Charutar Arogya Mandal
3Department of Tribal Development, Foundation for Diffusion of Innovations
4Department of Pediatrics, Pramukhswami Medical College
Background: Poor IYCF-practices increase the risk of malnutrition and poor developmental outcomes. Low literacy, poor socio-economic conditions, and missed opportunities for counselling in hard-to-reach, interior tribal villages may adversely influence IYCF-practices.
Objective: To assess impact of behaviour change communication(BCC) on IYCF-practices in 6-12M infants in tribal Gujarat, India
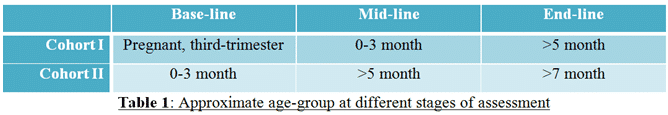
Design/Methods: Two blocks were randomly assigned to control(CC;N=541) and intervention(IC;N=474) clusters. Pregnant women in their third trimester(Cohort-1;N=610) and mothers of 0-3M infants(Cohort-2;N=405) were recruited in both clusters at baseline(N=1015) during Apr-Jul’16. Enrollee in the intervention group received interpersonal BCC for age-appropriate IYCF-practices (including discouragement of traditional, harmful feeding practices) at baseline, mid-line(Aug-Dec’16), and recipe demonstration and group counselling(Dec’16-Jan’17). End-line assessment(Jan-Mar’17) assessed the impact of BCC on maternal awareness and IYCF-practices.
Results: At baseline, maternal profile and awareness about IYCF-practices were similar in IC and CC. Lost-to-follow-up much higher than anticipated at end-line in CC and IC(228;48% vs. 299;55%) mainly attributed to out-migration. Being male(129;48.86% vs. 89;37.71%) and first child(70;52.24% vs. 148;40.44%) were significantly associated (p<0.02) with minimum meal frequency(MMF) for 6-8M and 9-12M infants. Minimum dietary diversity(MDD), i.e. infants receiving foods from four or more food groups, were similar(18;7.29% vs. 16;6.32%) in IC and CC. Among those who failed to achieve MDD, 35;14.17% and 29;11.46% in IC and CC received foods from three food groups, whereas 90;36.44% and 86;33.99% did not receive any complementary feeding in past 24 hours.
Conclusion(s): MDD practice improved during end-line compared to mid-line during which none of the infants in cohort-2 in IC and CC received meals from 4 or more food groups. However, both MMF and MMD remained sub-optimal over the course of the intervention assessment. While socio-economic status, food insecurity and migration could influence CF practices, further research is required to identify context-specific barriers and locally adaptable solutions to curb malnutrition in tribal population.
Powered by Eventact EMS