Background: Detection of axial disease involvement in patients with Psoriatic Arthritis (PsA) has important implications. Data on the structural changes of the spine and sacroiliac joints (SIJ) in PsA is mainly based on plain radiographs and MRI of SIJ. The prevalence and distribution of spinal changes as detected by MRI is largely unknown.
Objectives: To evaluate acute and structural changes in spine and SIJ by whole spine MRI performed in a consecutive clinical cohort of PsA patients.
Methods: Adult PsA (CASPAR criteria) patients were enrolled and underwent clinical exam, CRP, HLA-B27 tests, and MRI of the entire spine and SIJ (spinal sagittal T1-W, STIR and SIJ semi-coronal T1-W and T2-W with fat saturation sequences). The spine was scored for the presence of syndesmophytes, bone marrow edema (BME)/fatty corners and enthesitis. SIJs were scored (Berlin score) for the presence of BME, fatty replacement, erosions, sclerosis, and ankylosis. Findings were further categorized into active sacroiliitis (ASAS), structural sacroiliitis, and spinal findings compatible with PsA (≥3 BME or ≥4 fatty corners). All MRIs were evaluated by an experienced musculoskeletal radiologist, blinded to clinical data.
Results: Ninety six patients completed the study (average age: 50 years old, M:F: 50:46). Active/structural/total sacroiliitis was detected in 26%/11.5%/37.5% of patients, respectively. Spinal PsA was demonstrated in 15.6% (Table 1). Isolated spinal changes were detected in 2.1% of the cohort. Presence of inflammatory back pain (IBP) by ASAS correlated with the prevalence of active sacroiliitis (p 0.024) and PsA (axial/SIJ) (p 0.003). The extent of psoriasis severity (PASI) correlated with both SIJ and whole spine PsA changes. (p 0.02 for both) Gender differences or biologic therapy did not affect the prevalence of SIJ or spine involvement.
Table 1. Whole spine MRI findings.
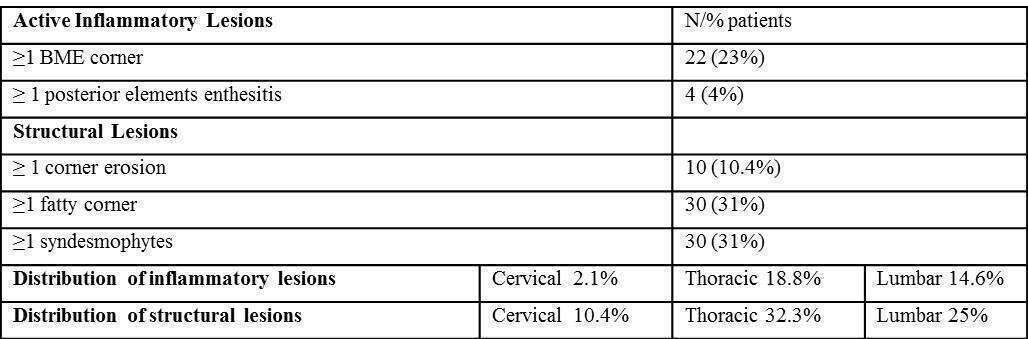
Conclusions: In the present PsA cohort, active and structural sacroiliitis was more prevalent vs typical spinal SpA changes. In particular, there was a paucity of PsA changes in the cervical spine. The most prominent axial findings included fatty corners and syndesmophytes. IBP presence and extensive skin disease correlated with PsA axial and SIJ changes.

