
The Value of Monocyte to Lymphocyte Ratio on Predicting the Early Prognosis of Patients with ST-Segment Elevation Myocardial Infarction Undergoing Primary Percutaneous Coronary Intervention
2Lithuanian University of Health Sciences, Kaunas
Background: Coronary atherosclerosis and plaque destabilization are the main causes of STEMI. White blood cells count(WBC), lymphocyte count(L), neutrophil to lymphocyte ratio(NLR),monocyte to lymphocyte ratio(MLR) have all been reported to be independent predictors of cardiovascular outcomes in patients with coronary artery disease.
Aim: investigate the association between early mortality MLR and other biochemical indices in patients with STEMI undergoing primary PCI (PPCI).
Methods: This study included 774 STEMI patients treated with PPCI who were analyzed in a retrospective study conducted in the hospital of the Lithuanian University of Health Sciences, Kaunas Clinics from 1st January 2014 to 1st January 2016. Patients were studied according to the presence of various demographic, logistic (pain to balloon time (PTBt)), clinical data, coronary artery angiography, transthoracic echocardiography, blood test results.
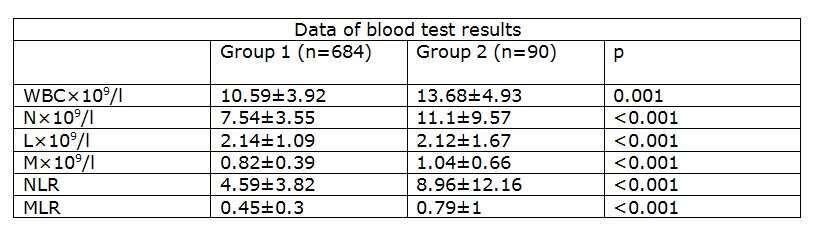
Results: Of the 774 patients studied 90 died at hospital (group1) and 684 survived (group 2). Group1 patients were older (78.48±10.5 yrs vs 66.24±12.6, p<0.001), with longer time from symptoms onset to hospital arrival more than 24 hours (40.7% vs 19.4% patients, p<0.001), more severe left ventricle dysfunction (LVEF 28.98±13.9% vs 40.86±9.2%, p<0.001), higher Killip class (15.4 % vs 6.6% with Killip III and 67% vs 5% with Killip IV),and with no reflow in 17.6% vs 9.3% patients, p=0.02, compared with group2 patients. While using multiple logistic regression analysis, it was found that in hospital mortality increased with age (OR 1.1; CI 1.05-1.15; p<0.001), LVEF (OR 0.92; CI 0.88-0.96; p<0.001), MLR (OR 4.9; CI 2.94-10.62; p<0.001),PTBt>24 hours(OR 4.2; CI 1.78-10.13; p<0.001).
Conclusion: An increased MLR ratio on admission is significantly associated with the in-hospital mortality rate of patients with STEMI undergoing PPCI.

Powered by Eventact EMS