Purpose: Evaluation of Superior vena cava syndrome (SVCS) with CT usually focuses on diagnosis of the condition, identifying the cause of obstruction and describing collateral pathways. While the contemporary literature discusses these features in small groups of patients, we sought to further describe the imaging characteristics of SVCS related to malignant causes in a large cohort.
Material & Methods: Retrospective review of chest CTs of 128 patients with SVCS. A radiologist with 4 year`s experience evaluated each of the following veins and structures: SVC, right and left brachiocephalic veins (RBcV, LBcV), right and left jugular veins (RJV, LJV), right and left subclavian veins (RScV, LScV), right atrium (RA), right ventricle (RV) and pulmonary arteries (PA). Degree of obstruction was classified as complete, near complete, partial or none. Type of obstruction was designated "invasion" in case of direct and irregular continuity of the tumor into the lumen. "External compression" was noted when tumor impressed or completely collapsed the adjacent vessel, without intraluminal irregularity. "Bland thrombus" was defined as a hypodense intraluminal filling defect which is not continuous with the tumor and is located in a synchronous site other than the level of the obstructing tumor. Collateral vessels, subcutaneous edema, skin thickening, pleural and pericardial effusions were also documented.
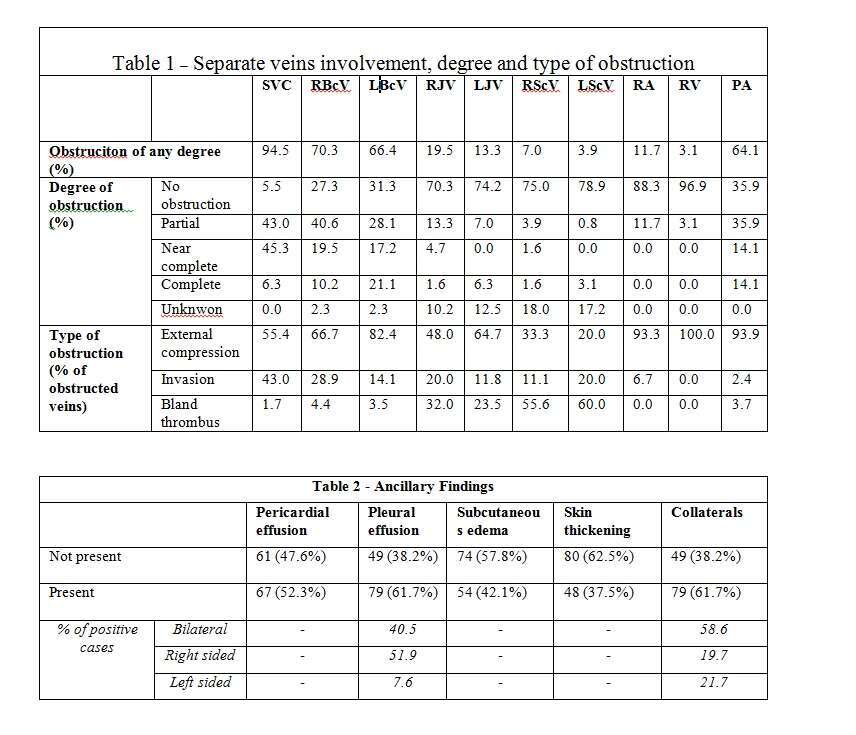
Results: Obstruction was more common in the SVC, RBcV and LBcV (94.5%, 70.3%, 66.4% respectively) than the RJV, LJV, RScV and LScV (19.5%, 13.3%, 7.0%, 3.9% respectively). Involvement of PA (64.1% of cases) was mostly due to external compression (77/82). Complete or near complete obstruction of at least one vein were noted in 43% and 38.3% of cases respectively, whereas in 18.8% of cases only partial obstruction was seen. In 21 cases (16.4%) there was evidence of a bland thrombus proximal to the site of tumoral invasion or compression, and separate from the tumor, 3 of which had concurrent pulmonary emboli.
In cases with pleural effusion, right sided effusion (51.9%) was more common than bilateral (40.5%) or left sided (7.6%) effusions. Bilateral collaterals (58.6%) were more common than unilateral ones (41.4%).
Conclusion: This is the largest cohort (n=128) describing CT characteristics of malignant SVCS. Obstruction of the SVC and primary tributaries was common, while the jugular and subclavian veins were less frequently obstructed. Nevertheless, the common involvement of pulmonary arteries (64.1%) and substantial incidence of synchronous bland thrombi (16.4%) highlights the extensive nature of SVCS beyond the level of obstruction.