Purpose: To identify the MRI characteristics of the prostate in a healthy population without clinically suspected prostatic carcinoma, that can be used as reference tool when screening for prostate cancer in specific high risk populations.
Material & Methods: Ninety eight asymptomatic BRCA carriers screened for prostate cancer, with normal PSA levels underwent mutliparametric MRI on a 3 Tesla machine. Lesions suspicious for carcinoma were biopsied and patients with proven cancer were excluded. The MRI studies were evaluated by two readers with 10 (reader 1) and 2 (reader 2) years of experience in abdominal imaging for overall dimensions, peripheral zone (PZ) thickness and signal, central zone (CZ) distinction from adjacent tissue, transition zone (TZ) texture and dominant nodules, seminal vesicles (SV) distention, signal and symmetry, conspicuity of capsule and the PZ/TZ border, and neurovascular bundle (NVB) delineation. A third radiologist used dedicated software to measure PZ and TZ volumes and ADC values of PZ and TZ.
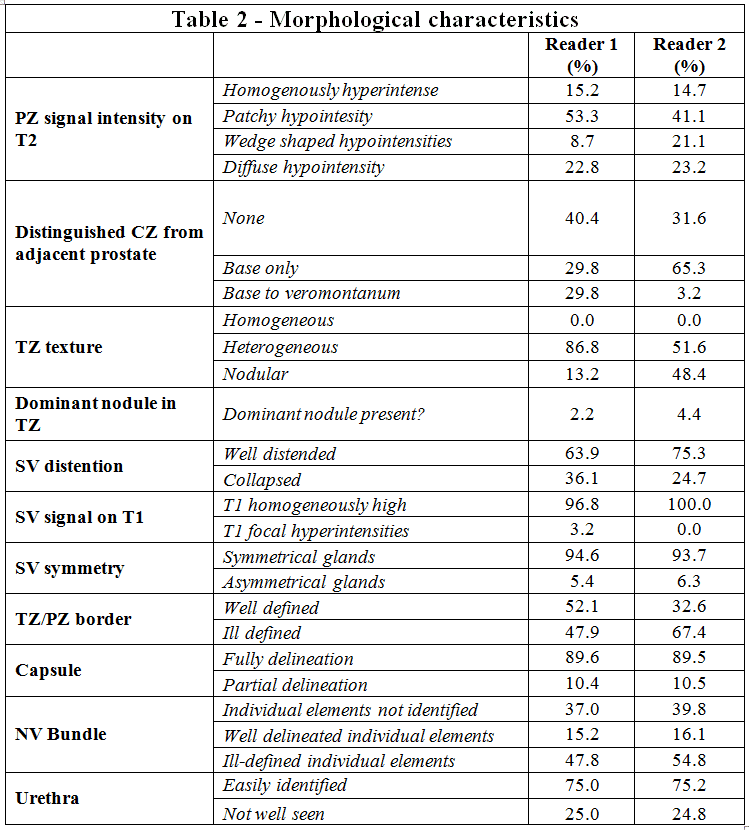
Results: Pulled average results for both readers showed homogenous or patchy T2 hypointensity in 70.2%, as opposed to previously reported homogenous T2 hyperintensity. Agreement was higher for the PZ pattern (78%) than the TZ texture (58%)This was partially due to a high proportion of examinations showing with tiny nodules described as nodular by reader 2 and heterogeneous by reader 1, and likely representing the normal sequelae of nodular hypertrophy. The central zone could be fully or partially distinguished from adjacent parenchyma in 64% of cases. The capsule was well defined in 89.5% of cases with good agreement (85%). There was poor agreement between readers regarding conspicuity of TZ/PZ border and NVB (62% and 48% respectively). Agreement on SV distention, T1 signal and symmetry was 78%, 92% and 86% respectively.
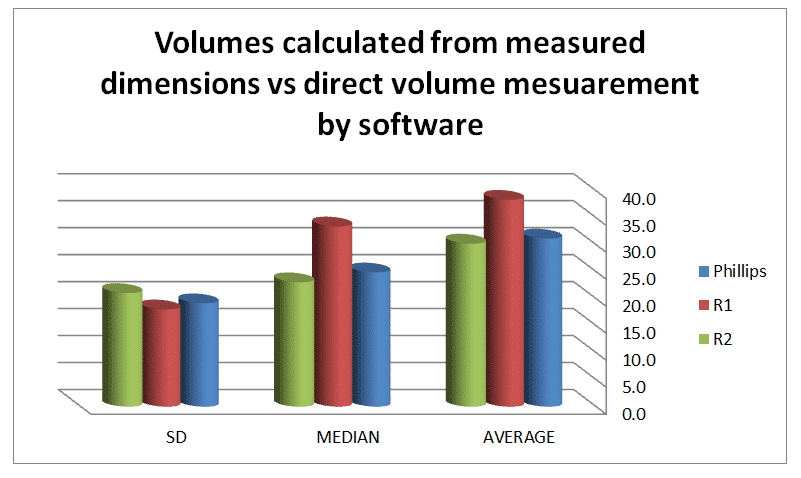
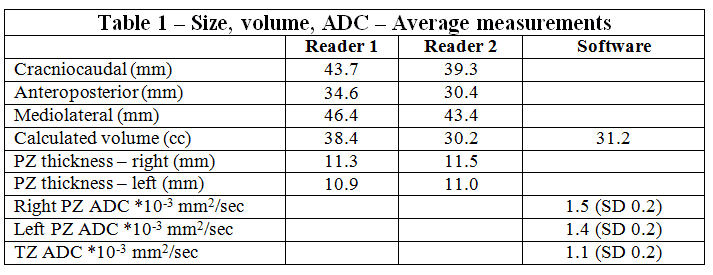
Results of objective measurements are shown in Table 1 and Figure 1. Subjective evaluations shown in Table 2.
Conclusion: In this cohort of healthy individuals, diffuse or patchy low T2 signal was a common finding in the PZ as opposed to sparse previously published data. Inter-reader variability was higher when classifying TZ texture and its border with the PZ, as compared to PZ signal classification, likely due to the development of a nodular pattern with time. We hope that additional data such as this will help as a reference tool when screening for prostate cancer in specific high-risk populations.