Purpose: Chronic pain is a major problem for individuals with spinal cord injury (SCI), affecting about 50% of the patients. Despite its clinical significance, the pathophysiology of the chronic pain following SCI remains largely unknown. In attempt to elucidate the neural underpinnings of the phenomenon, we undertook a Magnetic Resonance Imaging (MRI) study comparing brain structure and function between SCI patients with chronic pain, SCI patients without chronic pain, and healthy controls.
Materials and Methods: Thirty five individuals participated, consisting of 12 SCI patients with chronic pain, 5 SCI patients without chronic pain and 18 age-matched able-bodied controls. All the participants were males in order to eliminate gender effect. Subjects underwent a MRI scan, including structural and functional imaging sequences. In a functional MRI (fMRI) task, subjects were presented with alternating blocks of painful thermal stimuli at pre-adjusted relative intensities, delivered to their left forearm. Perceived pain ratings, were obtained using a 1-10 Visual Analog Scale (VAS) scored with the right hand.
Results: In our preliminary results, the task reliably activated brain regions associated with pain processing—primary and secondary somatosensory cortices, insula, cingulum, cerebellum, middle frontal gyrus, inferior frontal gyrus, and inferior parietal lobe—primarily in the right hemisphere, contralateral to the stimulated arm. However, no significant differences—neither in brain activations, nor in pain ratings—were observed between the three groups.
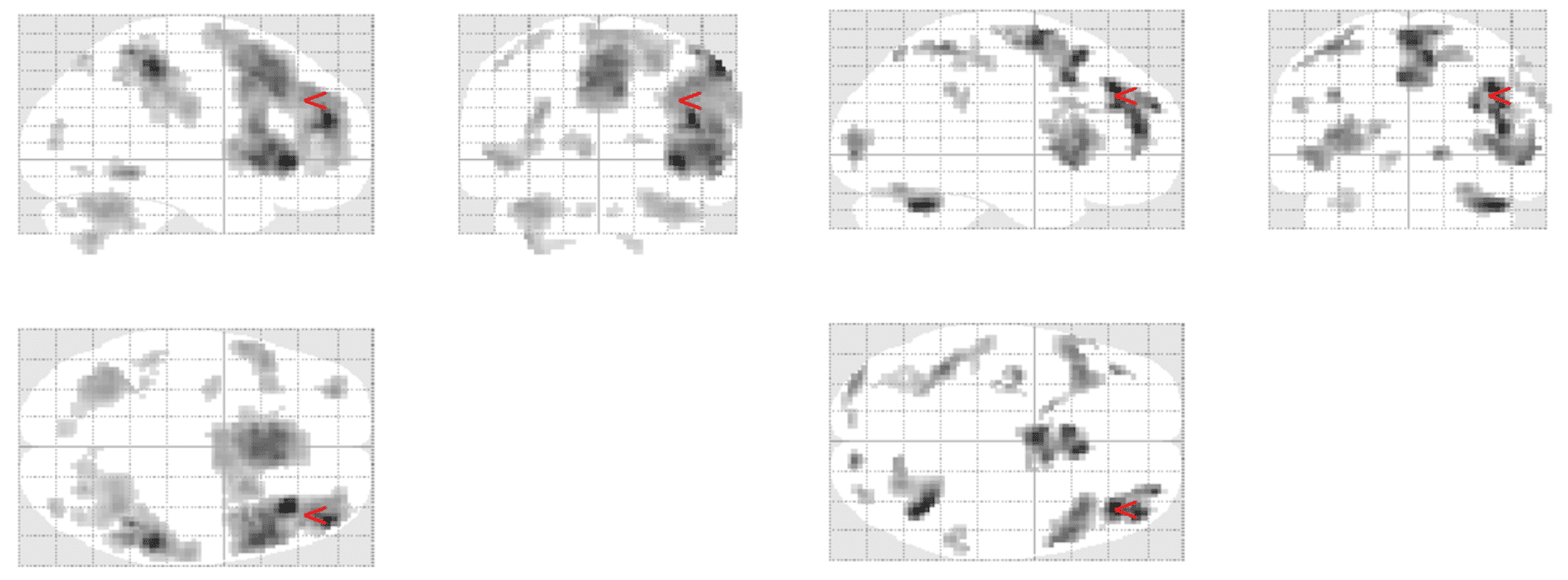
Figure 1: Brain activations in response to painful thermal stimuli in patients with SCI (Right) and in healthy controls (Left) (p
Conclusion: The results indicate that response to acute thermal pain, does not significantly differ between SCI patients and healthy controls, nor between SCI patients with and without chronic pain. The small sample size and the relatively moderate stimulation intensities used may underlie the lack of group differences. Alternatively, brain activation induced by experimental noxious stimuli may not represent the functional manifestations of chronic pain. Further study using larger samples and additional investigative techniques such as analyses of structural and functional brain connectivity, may advance our understanding of the neuropathophysiology of chronic pain following SCI.

