
Postpartum Tubal Ligation (PPTL) and Type of Anesthesia: How Successful are Our Neuraxial Interventions?
Background: Tubal ligation in the immediate postpartum period is typically performed on the L&D Suite. Use of an existing epidural catheter has been advanced as an efficient way to provide anesthesia. Reported epidural reactivation success rates vary from 74% to 92%. Predictors for failure include poor patient satisfaction with labor analgesia, increased delivery-to-reactivation time, and the need for top-ups during labor. Within our practice, some have suggested that labor analgesic epidurals activated for PPTL have a failure rate that does not justify leaving a catheter in place after delivery. We undertook this study to evaluate this claim and determine if there are predictors that can refine our anesthetic decision making.
Methods: After obtaining IRB approval, a retrospective chart review from July 2010 to July 2016 was conducted using CPT codes. Demographic data, obstetric data and anesthetic data were obtained.
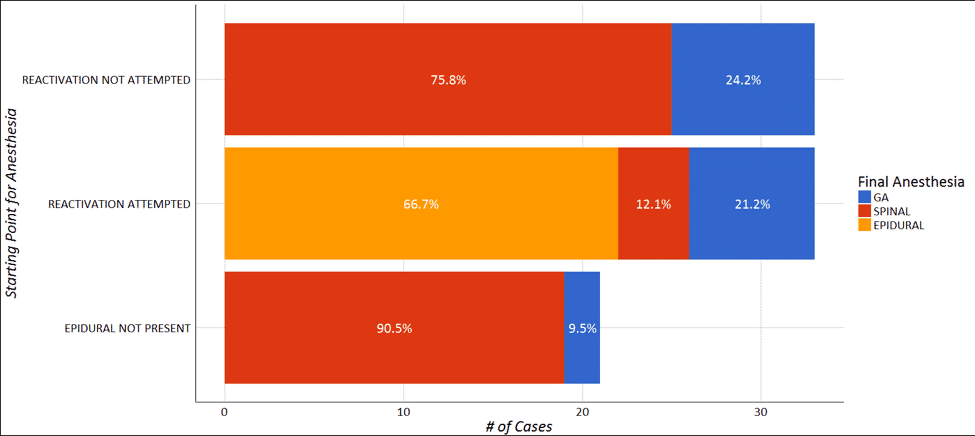
Results: Data from 93 patients were analyzed. 70 patients had labor neuraxial analgesia, and the reactivation success of epidural catheters was 66.7%. No demographic or anesthetic factors were predictive of failure to reactivate. Intrathecal fentanyl doses above 20 mcg added to bupivacaine were associated with spinal failure (p=0.001).
Conclusions: Our successful postpartum epidural reactivation rate for tubal ligation is lower than the range reported in the literature. We found no association between previously reported risk factors and unsuccessful epidural reactivation. The success rates for both spinal anesthesia and epidural reactivation for PPTL is lower than the reported 95% for cesarean delivery, reflecting a lower level of motivation on behalf of both the patients and anesthesia providers to tolerate suboptimal anesthesia when fetal considerations are removed.

Powered by Eventact EMS