
Clinical Factors Influencing Emergence Delirium in Pediatric Post-anesthetic Patients
2Intensive Care Unit, Assuta Medical Centers
3KPA,University of Turin, Italy and IDR, Hebrew University, Jerusalem, KPA
Background: Post anesthesia emergence delirium (PAED) can occur upon emergence from anesthesia. Emergence delirium (ED) may be distressing to the patient, parents, and caregivers, and can result in self-harm. The phenomenon is well-known since 1961 but only limited data is available regarding clinical factors which influence it.
Objective: The goals of this study are 1) Determine the incidence and severity of PAED; 2) Determine risk factors and possible mitigating factors
Methods: We analyzed the electronic database of an elective surgical hospital. During 2012-2016 28,386 pediatric patients (Age 0-15) underwent anesthesia for a variety of procedures. In the post anesthesia care unit (PACU) emergence delirium was assessed using a PAED score. We correlated clinical parameters to degree of delirium.
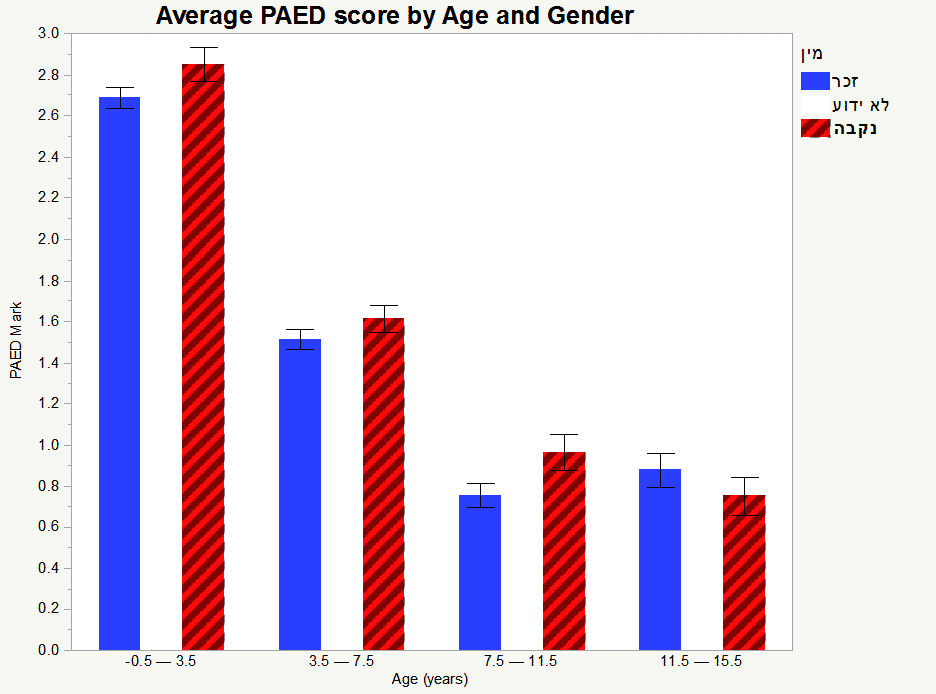
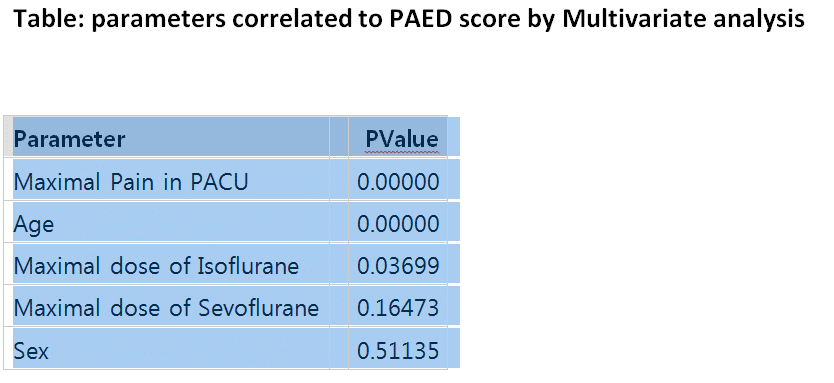
Results: ED was strongly related to patient`s age. Younger patients had more frequent and more severe PAED score. (Graph, Table)In addition, types of surgery, use of inhalational agents were also related to increase PAED score. Surprisingly, addition of regional techniques, such as caudal block, increased delirium as measured by the score. Use of opiates and Propofol decreased PAED score. Use of midazolam did not decrease PAED scores.
Conclusion: An ED phenomenon is an important challenge for physicians and nurses in PACU. Knowledge about the clinical causes for this may help clinicians and parents cope with the problem. Further studies are needed to assess the causal relationships and possible therapeutic approaches.

Powered by Eventact EMS