
Endothelial Progenitor Cells, Vascular Function, and Cerebrovascular Stroke
Background
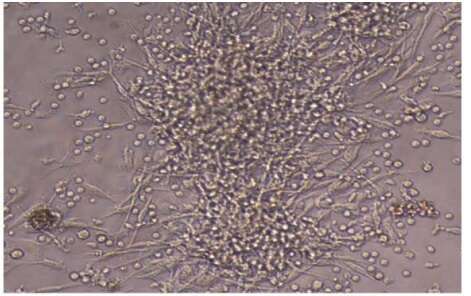
Cardiovascular risk factors contribute to cerebrovascular disease progression by inducing endothelial-cell injury and endothelial dysfunction. Endothelial progenitor cells may have a role in ongoing endothelial repair, and impaired mobilization or depletion of these cells may contribute to cerebrovascular disease progression. Our hypothesis was that endothelial progenitor cells contribute to regeneration of damaged endothelium in the cerebrovascular system. To test this hypothesis, the ability to grow in culture colony forming units of endothelial progenitor cells was studied as well as endothelial function of patients with ischemic stroke within the first 24 hours of symptoms onset.
Methods
We studied the number of colonies of endothelial progenitor cells (CFU-EPCs) of 22 male patients with stroke (58.09±9.8 years) and 13 healthy men (34±6.7 years), 8 female patients with stroke (54.6±10.3 years) and 6 health women (38.3±11.6 years). Endothelium-dependent function was assessed by high-resolution ultrasonography of the brachial artery, measured by flow mediated diameter percent change [FMD%] of the brachial artery. Peripheral blood was drawn soon after admission and was processed for endothelial progenitor cells in culture. For statistical analysis we used the students T-test Spearman`s test.
Results
Patients with stroke had a strong correlation between CFU-EPCs in culture and endothelial dysfunction (r=0.827, P<0.01). Male patients had endothelial dysfunction with FMD% of -2.2±9.7% vs. 17.5±6.8% in healthy males (p=0.0001), and female patients had FMD% of -7.2±10.1% vs. 25.1±7.1% in healthy females (p=0.0001). Men with stroke had 5.5±6.3 CFU-EPCs vs. 23.75±5.3 (healthy males) (p=0.0001), women with stroke had 7.6±4.9 CFU-EPCs vs. 22.25±6.7 (healthy females) (p=0.0004).
Conclusions
Patients with acute stroke had an impaired ability to grow CFU-EPCs in culture and endothelial dysfunction. Inability to grow colonies of endothelial progenitor cells reflects the impaired regenerative capacity of patients with cerebrovascular disease and may partly explain the development of cerebrovascular disease.
Powered by Eventact EMS