
Ability of Short-Term Risk Mortality Scores to Predict Long-Term Survival in Patients Undergoing Cardiac Surgery
Objective
The Society of Thoracic Surgeons Predicted Risk of Mortality score (STS PROM), EuroSCOREI (ES1) and EuroSCOREII (ES2) reliably predict 30-day mortality after cardiac surgery. Data on the ability of these short-term indices to accurately predict long-term survival are sparse. We sought to assess the ability of STS PROM, ES1 and ES2 to predict long-term survival.
Methods
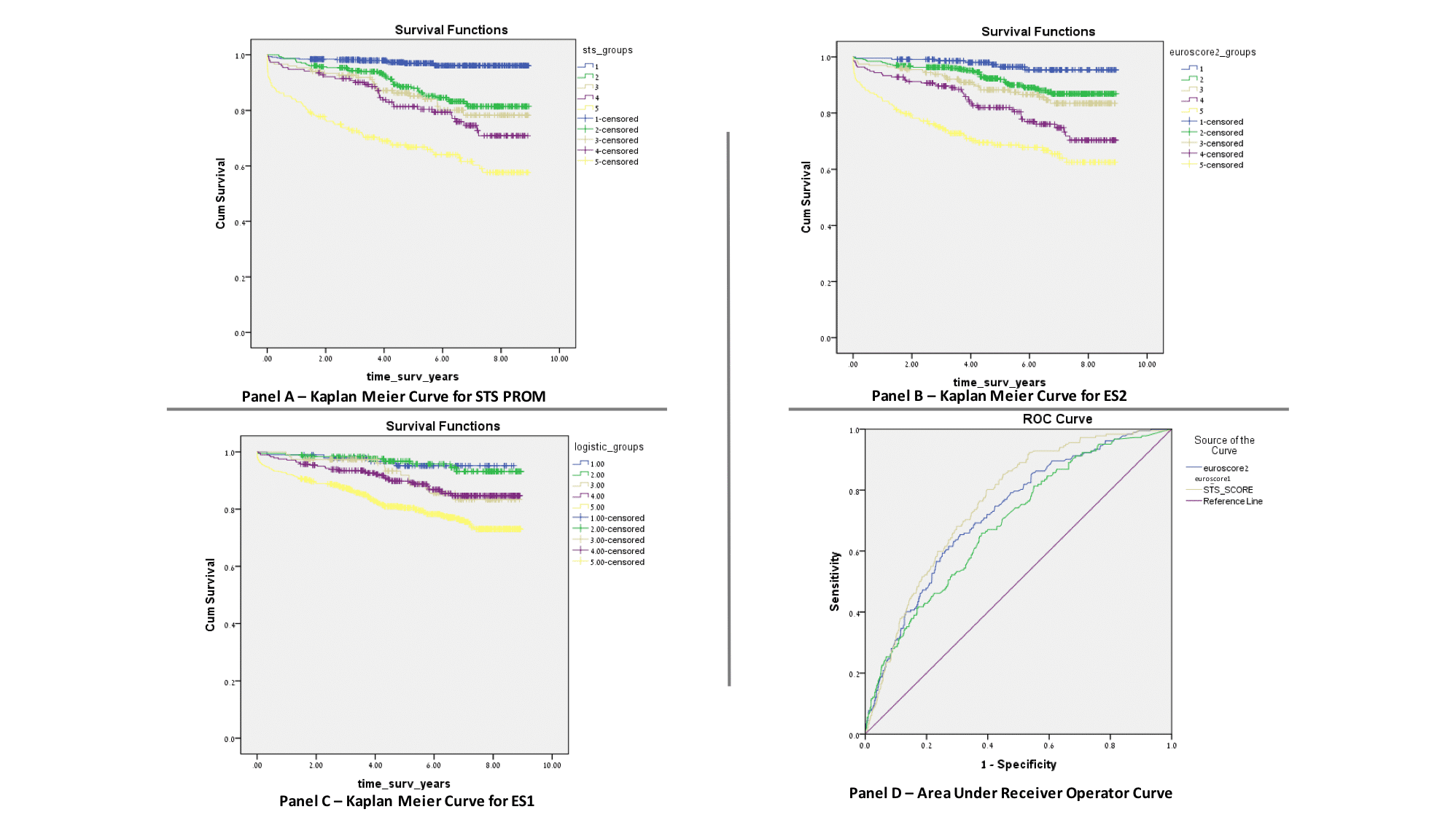
Demographic, clinical and procedural data on 1279 consecutive patients undergoing any of 5 cardiac operations with a calculable STS PROM were prospectively collected and used to calculate STS PROM, ES1 and ES2. Patients were stratified into 5 risk-score categories based on their scores (1: 0-0.99%, 2:1.0-1.99%, 3: 2.0-2.99%, 4: 3.0-4.99%, 5: >5%). Long-term survival data were obtained from the National Death Registry. Kaplan-Meier (KM) survival curves were plotted for each risk-score category and compared using Log-rank test. Model discrimination was assessed using the Area Under the Receiver Operating Curve (AUC). We used Cox regression analysis to identify independent predictors of long-term survival.
Results
Mean follow up was 62±28 months (range 1-107 months). Mean survival of the entire cohort was 95±1 months. Long-term survival was inversely related to the STS-PROM, ES1 and ES2 (Panels A, B and C). STS PROM and ES2 predicted long-term survival more reliably than ES1. Eight-year survival for the 5 STS risk-score categories was 96±1%, 81±3%, 78±4%, 70±5%, 57±4%, respectively (p<0.0001). STS PROM model discrimination (0.76±0.02) exceeded that of the ES1 (0.69±0.02) and ES2 (0.72±0.02) (Panel D). Cox regression identified age, incidence of surgery, diabetes mellitus, dialysis and STS PROM to be independent predictors of long-term mortality.
Conclusion
The STS PROM is a more reliable predictor of long-term survival in patients undergoing cardiac surgery compared to the ES1 and ES2. Mortality scores should be used in the discussion of long-term outcomes with patients and in the analysis of procedural cost-effectiveness.

Powered by Eventact EMS