Background Hepcidin is master regulator of iron metabolism. It has been shown that vitamin D suppresses hepcidin expression. Our aim was to examine the association between hepcidin, vitamin D and anemia in children with IBD.
Methods A prospective study was performed on naïve, newly diagnosed IBD patients. Control group consist of healthy children. Mild IBD patients were treated with 4000 unit of vitamin D, daily, for 2 weeks. Between- and within-group differences in iron biomarkers, 25-hydroxyvitamin D (25(OH)D), inflammatory markers (CRP, IL-6, Hepcidin) and hemoglobin concentrations at baseline and 2 weeks were determined.
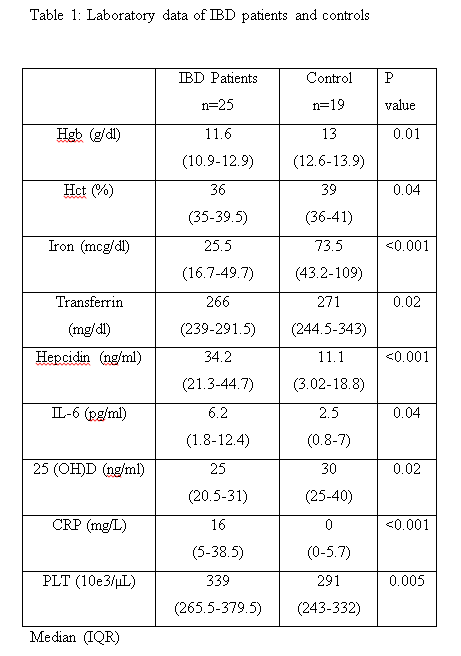
Results Forty- four children (25 IBD patients and 19 controls, 59% female /41% male, mean age 12.9±3.7 years) were recruited. At baseline, serum concentrations of hepcidin were significantly higher and 25-OHD, iron and hemoglobin were significantly lower in IBD patients compared to controls (34.2 ng/ml, 25 ng/ml, 25.5mcg/dl, 11.6 g/dl compare to 11.1 ng/ml,30 ng/ml, 73.5 mcg/dl, 13 g/dl, respectively p<0.05). Eleven children were treated with 4000 unit of vitamin D. After 2 weeks plasma hepcidin concentration decreased by 70.7%, CRP decreased by 83% and vitamin D increased by 17% (p-0.003, 0.005, 0.005 respectively).
Conclusion Hepcidin is involved in the pathogenesis of iron restrictive anemia in children with IBD. High dose vitamin D treatment increased CRP, IL-6, Hepcidin levels and showed a trend to increase iron levels within 2 weeks. We suggest that vitamin D may have a role in regulating iron recycling by change in pro-inflammatory markers.