
New-Onset (De-Novo) Acute Heart Failure Versus Acute Decompensated Chronic Heart Failure: Differences in Early Intermediate and Long-Term Mortality
Background and purpose: According to the present data it is unclear how hospitalized patients with acute heart failure who are previous long-term chronic Heart failure survivors (ADCHF) differ from those with new-onset (de-novo) acute Heart failure (AHF). Therefore, our aim is to assess the differences in early, intermediate, and long-term outcomes between hospitalized patients with AHF who are ADCHF and those with de-novo AHF.
Methods: we analyzed data of 2328 patients with acute heart failure, who were enrolled in the heart failure survey in Israel (HFSIS). The study patients were classified into de novo AHF and ADCHF. Multivariable analysis was used to determine the association between HF type and 1-year and 10-year all-cause mortality.
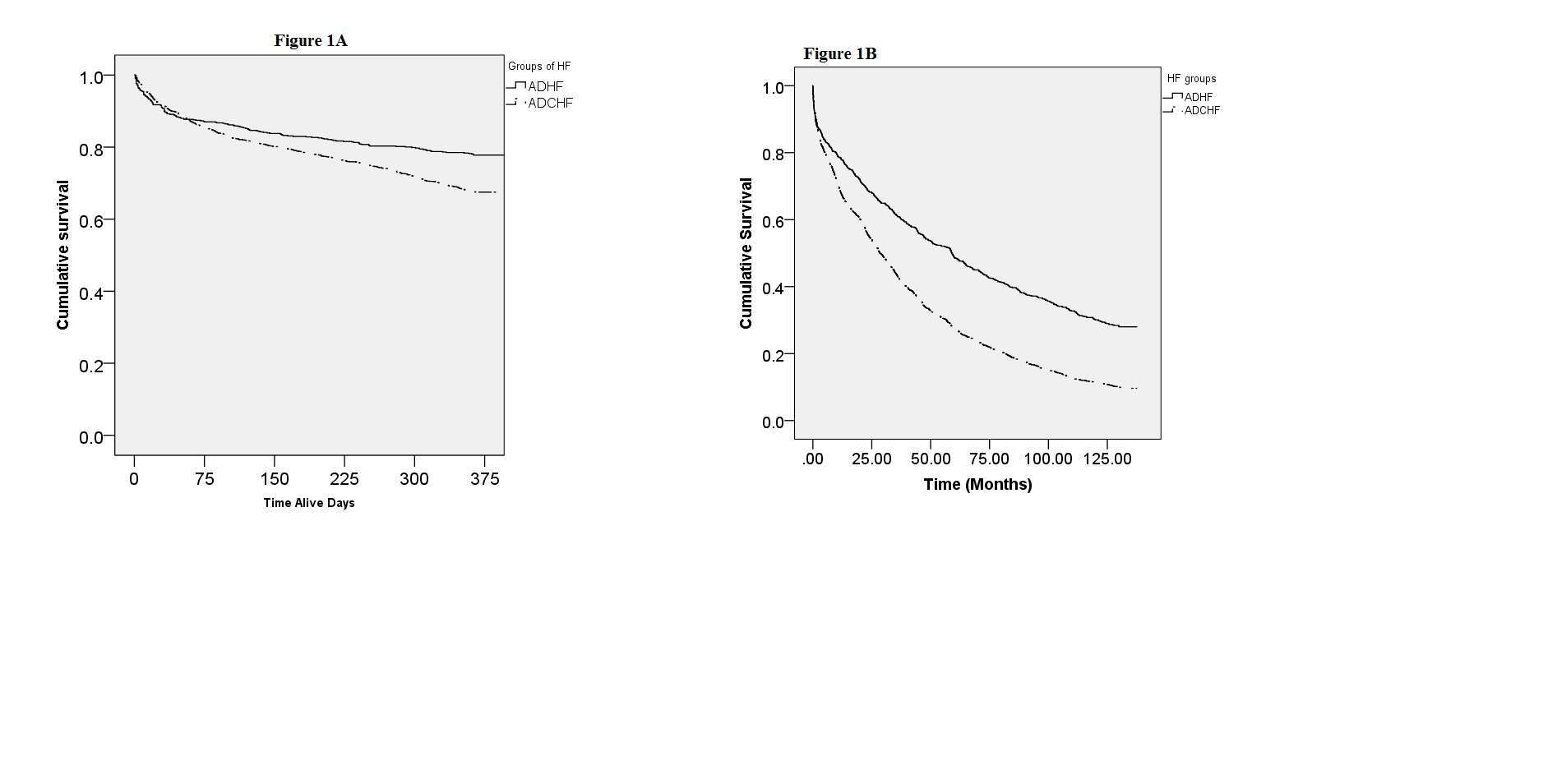
Results: 721(31%) patients were classified as de novo AHF, 1607 (69%) patients were classified as ADCHF. At 30 days mortality rates were similar among both groups (9% among de-novo AHF, 8% among ADCHF). Survival analysis showed that at 1 year the rate of all-cause mortality was significantly higher among patients with ADCHF ( 33%) compared to those with de-novo AHF (22%); (log rank P<0.001). similarly at 10 year all-cause mortality rates among patients classified as ADCHF were (90%), whereas among those with de-novo AHF (72%); (log rank P<0.001).
Consistently multivariable analysis showed that compared to patients with de-novo AHF, patients with ADCHF had an independently 58% and 48% , higher mortality risk at 1and 10 year of follow-up respectively, ( 1 year HR= 1.58;95%CI 1.05-2.38,P=0.03; 10 year HR= 1.48;95%CI= 1.23-2.77;P<0.001).
Conclusions: The long term prognosis after hospitalization for AHF is poor, with a significantly different survival observed in patients with de-novo AHF compared to ADCHF. A previous history of heart failure is an independent predictor of 1year and 10 year mortality. Distinction between ADCHF and de-novo AHF may improve our understanding of patients with AHF.

Powered by Eventact EMS