
Incidence, Predictors and Prognostic Implications of Dyspnea at Admission Among Acute Coronary Syndrome Patients Without Heart Failure
Background: Among patients with stable coronary artery disease, effort related dyspnea is associated with larger ischemic territory and worse outcome. Whether dyspnea, not related to heart failure, is also associated with adverse outcome among patients with acute coronary syndrome (ACS) has not been fully elucidated.
Methods: We studied all ACS patients enrolled in the biennial Acute Coronary Syndrome Israeli Surveys (ACSIS) during 2010-2013 who were classified as Killip I. Baseline characteristics, utilization of coronary interventions and outcome were compared between patients with chest pain only (n=2027) and those with chest pain + dyspnea (n=417).
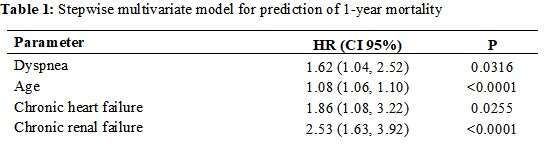
Results: ACS patients presented with dyspnea were older (64.4±13 vs. 61.8±12, p<0.001), less frequently men (75% vs. 81% p<0.001) and had higher rates of multiple comorbidities. Statistically significant predictors for dyspnea as a presenting symptom were female gender [HR 1.45 (1.11, 1.89)], chronic renal failure [HR 1.81 (1.30, 2.52)], chronic obstructive pulmonary disease [HR 1.59 (1.045, 2.429)] and angina ³24 hours [HR 1.46 (1.147, 1.86)]. Patients presenting with dyspnea were less likely to undergo primary reperfusion (31% vs. 42%, p<0.001) and less likely to undergo coronary angiography during their hospitalization (90% vs. 94%, p=0.002). Mortality rates were significantly higher among patients presented with dyspnea both at 30-day (3% vs. 2%, p=0.017) and at 1-year follow-up (9% vs. 4%, p<0.001). Dyspnea was found as an independent predictor of outcome (Table 1).
Conclusion: The presence of dyspnea is frequent and associated with adverse outcome among patients with ACS without signs of heart failure. Identification of this higher-risk cohort of patients is important and intensified treatment and closer follow-up may be warranted.

Powered by Eventact EMS