
The Outcome of Patients Admitted for Acute-Coronary Syndrome During “Off-Hours”
Introduction: Conflicting evidence exist regarding the outcome of patients admitted for acute-coronary syndrome (ACS) during regular working hours (RWH) versus those admitted after hours (“off-hours”-OH). We explored the outcome of ACS patients admitted during RWH and compare them to those admitted OH. We further compared between the outcome of patients admitted during and after hours of patients presented with ST-elevation myocardial infarction (STEMI) and non-STEMI (NSTEMI).
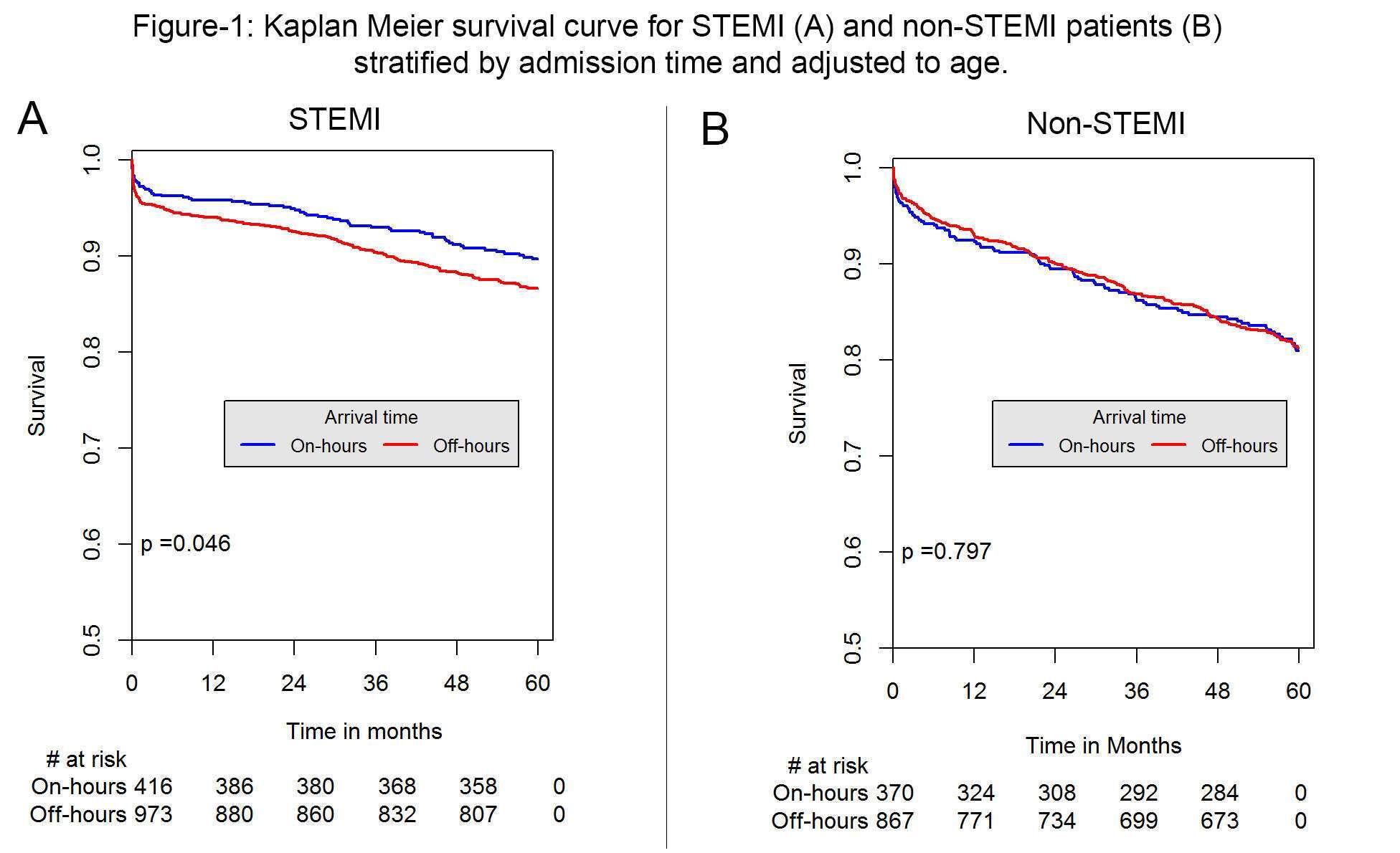
Methods: All patients included in the ACSIS survey between 2008-2016 were included. The baseline characteristics, therapeutic interventions and outcome were compared between patients admitted during RWH versus those admitted OH (including weekend and holidays). Subgroup analysis included Kaplan Meier 5-year survival comparison in patients admitted on versus OH in STEMI and non-STEMI patients.
Results: Of a total of 6,899 patients, 4,752 (68.8%) were admitted OH. Compared with those admitted DWH, patients admitted OH were younger (63.50±13 vs. 64.38±12.71;p<0.005) with similar incidence of diabetes mellitus and hypertension (38.4% vs. 40%;p=0.2, 63.4% vs. 64.7%;p=0.3 respectively). Although the time for reperfusion was longer in patients admitted OH (70.00 [IQR 40.00, 110.00] vs. 46.00 [IQR 25.00, 85.00] hours ;p<0..05), no difference was noted in 5-year all-cause mortality (20.9% vs. 19.8%;p=0.52). Subgroup comparison of 5-year survival demonstrated that while no difference in survival between non-STEMI patients admitted on versus OH, a significant difference in outcome was recoded in STEMI patients admitted OH (Figure-1).

Powered by Eventact EMS