
Frailty in Community-Dwelling Elderly in Israel and Long-Term Mortality Risk
Background: Frailty, a multidimensional syndrome of increased vulnerability to stressor events, is one of the most challenging expressions of aging. Frail individuals have an increased risk of mortality, disability and institutionalization. We developed a frailty index (FI) based on data of a national survey of Israeli elderly, and assessed its predictive value for all-cause and cardiovascular disease (CVD) death.
Methods: Data of the first National Health and Nutrition Survey of the Elderly (“Mabat Zahav”), conducted in 2005-2006 (n=1,799; mean age, 75 years; 52% women), were used to develop a FI based on accumulation of deficits. The FI was derived from 33 variables identified and scored according to published criteria, including self-rated health, functional limitations, comorbid conditions, cognitive function and weight loss. Follow-up lasted through 2017 for all-cause mortality and through 2015 for cause-specific mortality via the National Death Registry. Cox regression models were constructed to assess the association of FI with death, overall and by underlying cause (categorized as CVD vs non-CVD).
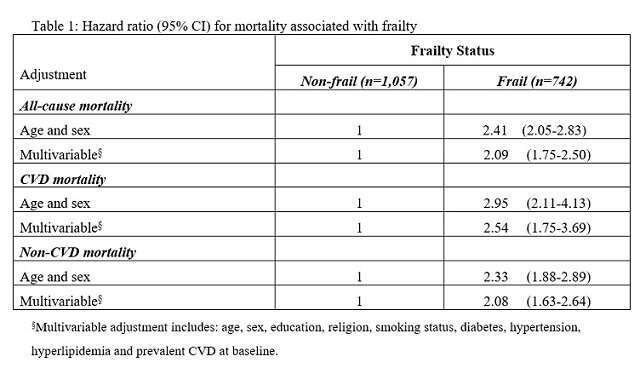
Results: Applying a standard threshold (FI ≥0.25), 41% (n=742) of subjects were classified as frail at baseline. During a mean follow-up of 9 (SD, 3) years, 684 subjects died. Frail participants had about two-fold increased risk for all-cause mortality and two and a half-fold increased risk for CVD mortality (30% of all deaths). Multivariable adjustment for a variety of demographic, socioeconomic, and clinical variables did not change the association materially (Table). Excluding subjects with prevalent CVD at baseline, the adjusted hazard ratios (95% CIs) were 2.20 (1.78-2.72) for all-cause death and 3.30 (2.05-5.30) for CVD death.
Conclusions: Frailty, calculated via an index of deficits, was associated with a substantial increase in mortality overall, and CVD mortality in particular, among Israeli elderly. Early and accurate identification of frailty may thus indicate which individuals will benefit most from preventive interventions.
Powered by Eventact EMS