
Real-Life Outcomes of Diabetic Patients Undergoing Surgical or Percutaneous Revascularization for Multi-Vessel Coronary Artery Disease
Background: Diabetes mellitus (DM) in patients with multi-vessel coronary artery disease (CAD) provides a poorer prognosis. While the main strategy for myocardial revascularization in these patients is by coronary artery bypass grafting (CABG), percutaneous coronary intervention (PCI) is being used with increasing frequency in many centers. We aimed to explore real-life clinical outcomes of patients with DM who were referred for coronary revascularization.
Methods: This prospective study include 1063 consecutive patients with multi-vessel CAD enrolled between January and April 2013 from all 22 hospitals in Israel that perform coronary angiography and PCI. Revascularization strategy was at the discretion of the treating team. Patients were followed-up for 3-years.
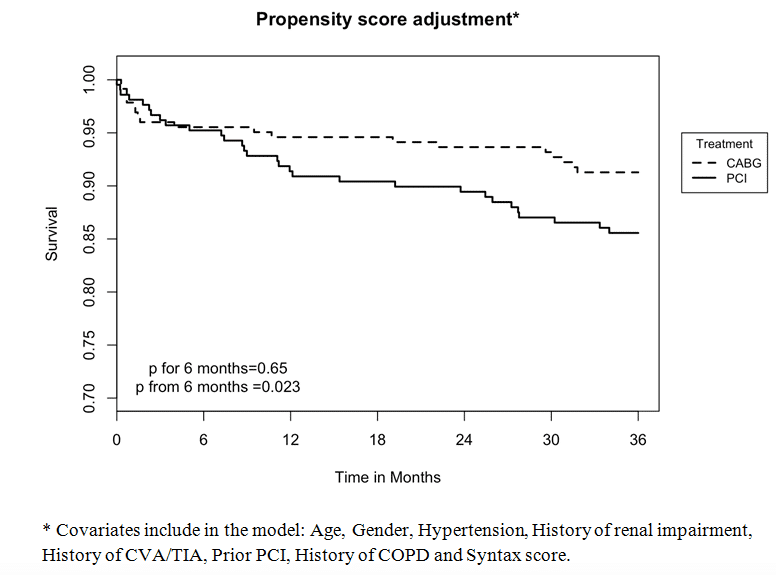
Results: From 1063 patients with multi-vessel CAD, 475 (45%) had DM. Of them, 48% were treated by CABG and 52% by PCI. Patients who were referred to CABG had higher rates of left main stenosis (36% vs. 12%, p<0.001) reflected by a higher mean SYNTAX score (28±9 vs. 18±8, p<0.001), more smokers (28% vs. 20%, p=0.074) and more males (77% vs. 65%, p=0.005), however less patients with renal impairment (13% vs. 20%, p=0.033) and prior PCI (33% vs. 45%, p=0.013). Factors associated with referral for PCI included: older age (OR=1.03; p=0.022), renal impairment (OR=1.94; p=0.036), prior PCI (OR=1.87; p=0.008), absent of left main stenosis (OR=1.85; p=0.039) and lower Syntax score (OR=1.15; p<0.001). Surgical revascularization revealed late survival advantage that have been seen from 6 months after revascularization and thereafter (Figure). Multivariable analysis showed that PCI was associated with an increased hazard for late mortality compared with surgical revascularization (HR=1.94 [95%CI 1.02-3.69]; p=0.005).
Conclusion: In real life practice CABG provides better 3-year outcomes compared to PCI in patients with DM.

Powered by Eventact EMS