
Neutrophil to Lymphocyte Ratio Is Associated with Increased Risk of New Atrial Fibrillation among Asymptomatic Middle Age Adults
Background: Clinical and experimental data support a critical role for inflammation in cardiovascular disease. The purpose of the current study was to examine the relation between neutrophil-to-lymphocyte ratio (NLR), a general inflammatory marker, and incident atrial fibrillation (AF) in large observational cohort.
Methods: We investigated 21,303 men and women who were annually screened in a tertiary medical center. All subjects were free of AF at baseline and had their serum NLR calculated based on their blood count at the first annual visit. Subjects were divided into two prespecified groups based on their baseline NLR: Low (<2.55; N=15,066 – 75%) and high (≥2.55; N=5,936 – 25%). The primary endpoint was new onset AF during follow-up.
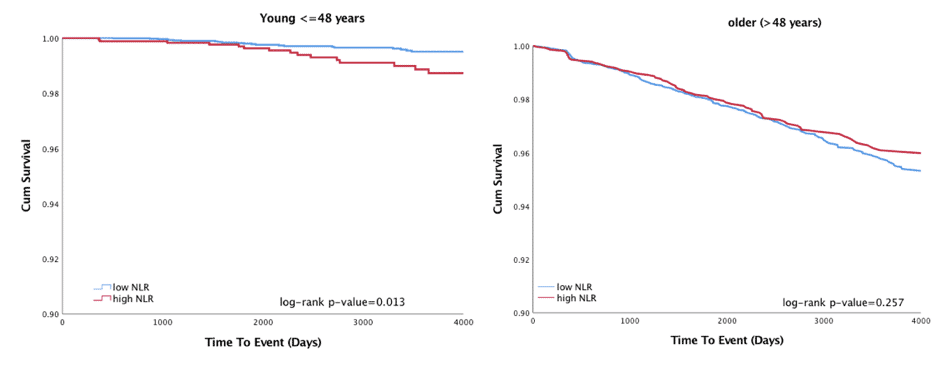
Results: Mean age of study population was 48 ± 10 years and 72% were men. A total of 373 (1.8%) incident events occurred during an average follow-up of 7.5±5 years. Unadjusted cox regression analysis demonstrated that each 1 unit increase in NLR was associated with a significant 10% increase in risk of occurrence of a first AF event (95% CI [1.003-1.22], p=0.043). Subgroup analysis showed that NLR-related risk was age-dependent, such that in the younger age-group (<=48 years) high NLR group showed a significantly higher event rate compared with low NLR group (Figure: right panel) whereas among older subjects the rate of events was similar between both NLR groups (Figure: left panel; p for interaction = 0.008). Multivariate cox regression analysis among younger subjects, with adjustment for age, gender, obesity, hypertension and diabetes mellitus, showed that subjects with high NLR were more than twice as likely to develop new onset AF during follow up compared with subjects with low NLR (HR=2.28, 95% CI [1.19-4.37], p=0.013).
Conclusions: Our findings suggest that high NLR is associated with increased risk of new onset AF. This finding is more pronounced among young adults.

Powered by Eventact EMS