
Transcatheter Aortic Valve Implantation Futility Risk Model: From the 4-Sites Israeli TAVI Registry
Background: Transcatheter aortic valve implantation (TAVI) risk assessment is still developing and mostly concerned in the peri-procedural period. We sought to develop and then validate the score parameters in the Israeli cohort.
Methods: This study comprised patients in the Israeli TAVI registry across 4 centers that underwent TAVI for severe aortic stenosis and had available data. We excluded patients with unsuccessful/sub-optimal implantation as defined by the VARC-2. The cohort was split to derivation and validation cohorts by a ratio of 70:30. We examined various demographic data, clinical details, echocardiographic and laboratory findings. The outcome was defined as 1-year composite of mortality, stroke, and no improvement in NYHA class (vs. baseline). Logistic regression was used to fit the prediction model.
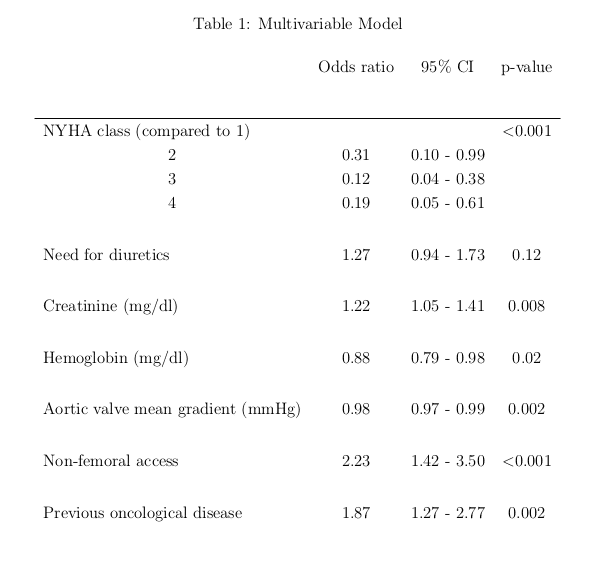
Results: Out of 2464 patients who met inclusion criteria, 276 (11%) have been excluded for unsuccessful/sub-optimal implantation, leaving 2188 patients that were split to 1532 in the derivation and 656 in the validation cohort. Mean age was 82 (±6.4) years and 54% were female. At one year, 299 (14%) patients experienced the adverse futility related outcome. The final model included mean AV gradient, use of diuretics, baseline functional class, hemoglobin and creatinine levels, and access site and previous oncological disease )Table 1). The model’s area under the curve (AUC) was 0.69 in the derivation and 0.68 in the validation cohort. Performance of other scores in the validation cohort was lower (0.55 for STS, 0.53 for Euroscore2, 0.57 for JACC, 0.55 for France2). Using the score and dividing patients into 3 risk category groups, produced a low risk (20/267, 7% futility), a medium risk (49/359, 14%) and high risk (18/43, 42%) groups.
Conclusions: the TAVI futility risk model can be used to provide further insight regarding prediction measures and/or patients` outcomes outside of the peri-procedural period.

Powered by Eventact EMS