
Frequency and Characteristics of Patients with Severe Lead-Associated Tricuspid Regurgitation: Is the Device Lead the Only Mechanism of Tricuspid Regurgitation?
Background and Objectives: Device leads crossing the tricuspid valve (TV) (pacemaker or defibrillator leads) are currently recognized as an important cause of tricuspid regurgitation (TR). However, it is unclear whether mechanical interference to the TV by the lead is the only mechanism of TR in patients with devices. The objectives of our study were: 1) to determine the frequency of lead-associated TR (LA-TR) among patients with severe TR; 2) to describe the characteristics of patients with severe LA-TR.
Methods: The transthoracic echocardiography reports of consecutive patients with severe TR, who were examined at our institution during a 20 months period, were reviewed. The characteristics of patients with LA-TR were compared to those without a lead (non-LA-TR).
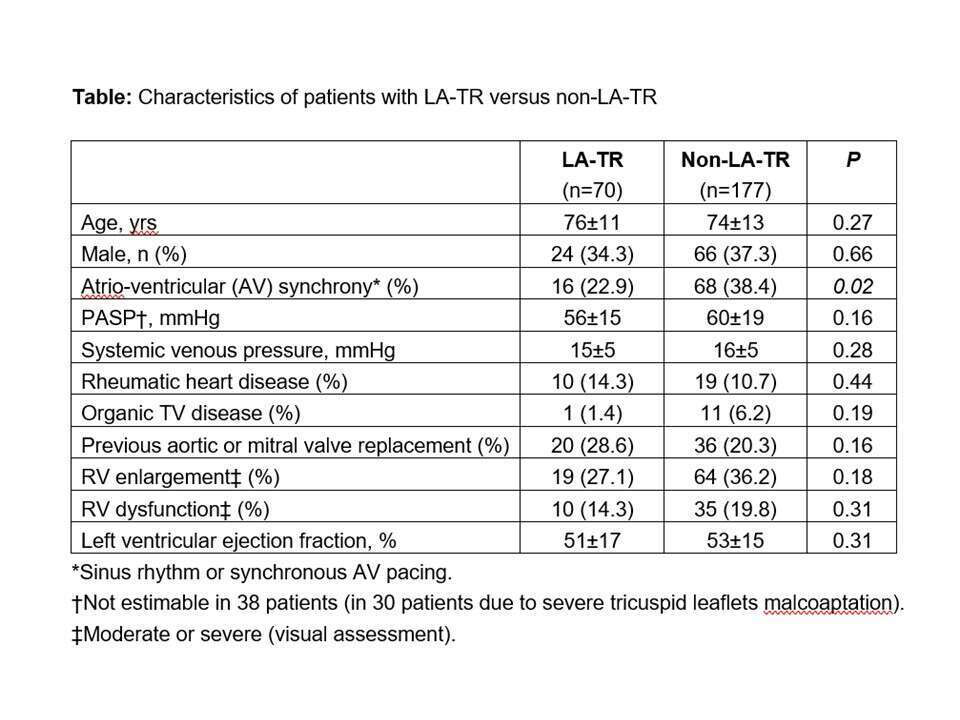
Results: During a 20 months period, 247 patients with severe native valve TR were identified: 70 (28.3%) were LA-TR and 170 (71.7%) were non-LA-TR. The Table compares the characteristics of patients with LA-TR to those with non-LA-TR. The frequency of multiple established risk factors for TR [advanced age, elevated pulmonary artery systolic pressure (PASP), rheumatic heart disease, organic TV disease, and right ventricular (RV) remodeling] were similar in the 2 groups. Atrio-ventricular (AV) synchrony was less common in LA-TR.
Conclusions: The frequency of LA-TR is high among patients with severe TR (~ 30%), thereby confirming the association between the presence of a device lead and severe TR. Nevertheless, the frequency of non-lead risk factors for TR was similar in patients with LA-TR and non-LA-TR and AV dyssynchrony was even more frequent in LA-TR. These findings suggest that non-lead risk factors play an important role in the pathogenesis of TR in LA-TR, in addition to the device lead itself.
Powered by Eventact EMS