
The Vicious Cycle of Dyspnea and Heart Failure
Introduction: Heart failure (HF) is characterized by decompensation phases. We hypothesized that (1) decompensation results into dyspnea, mainly due to increased respiratory effort; (2) dyspnea degree can be quantified by respiratory effort severity; (3) increase in respiratory effort causes further heart failure deterioration.
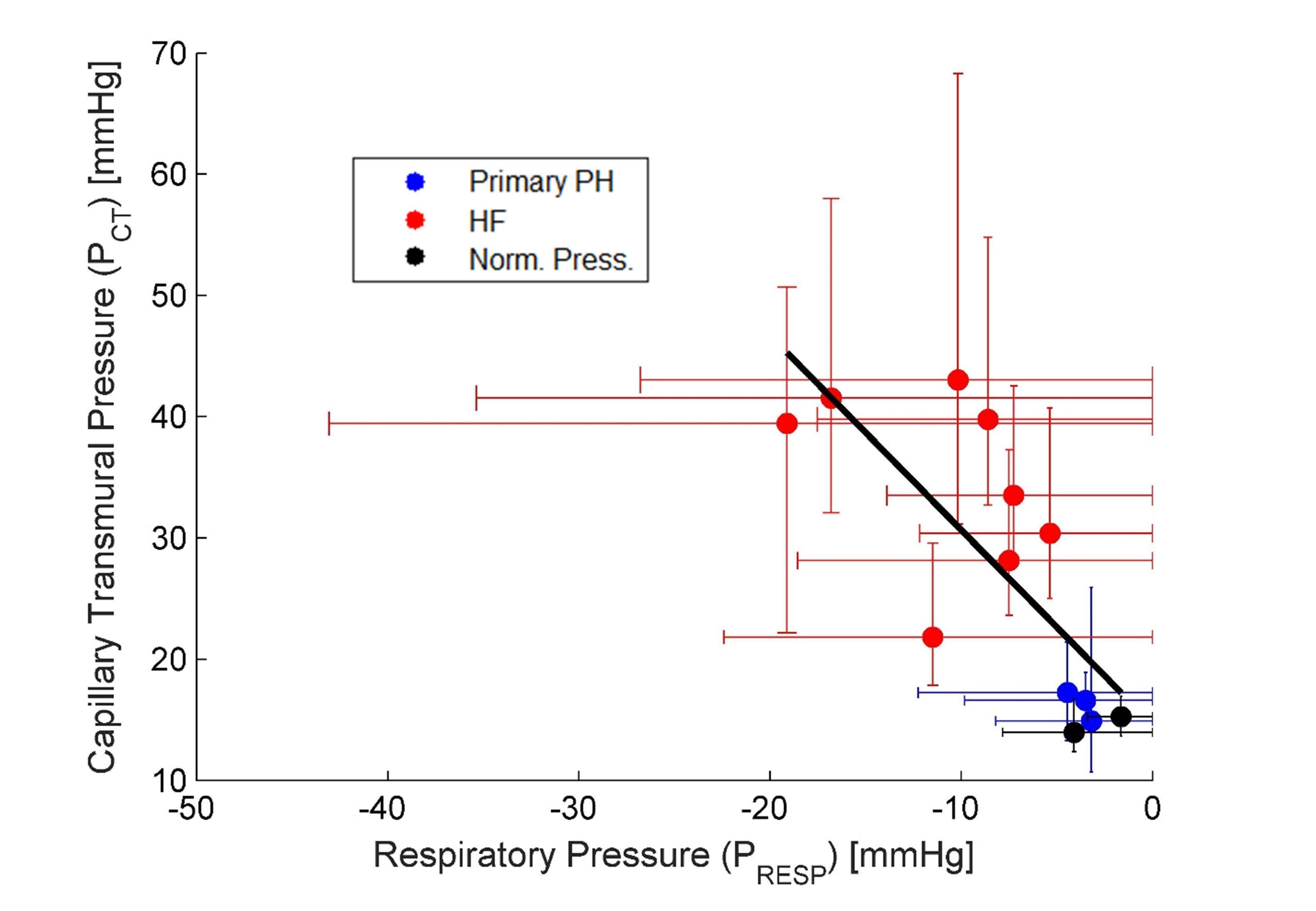
Methods: The study enrolled a total of 13 patients undergoing right-heart catheterization to clarify dyspnea diagnosis. Additionally to the standard parameters, measurements of respiratory flow and chest wall dynamics were obtained using facial mask and three motion sensors. Pulmonary wedge pressure was separated into two waves: the respiratory wave (PRESP) and the capillary transmural pressure (PCT).
Results: According to right-heart catheterization, 3/13 patients had primary pulmonary hypertension, 8/13 left-sided HF (preserved or reduced) and 2/13 had no evidence of pulmonary hypertension. Remarkably, PRESP values were very high - up to 43 mmHg in HF patients, and there was high correlation between PRESP (surrogate of dyspnea) and PCT (r = 0.76). Namely, every 1.6 mmHg elevation in PRESP corresponded to 1 mmHg increase in PCT. This raises the question of cause/consequence relationships. An increase in the wedge-pressure increases pulmonary capillary pressure, leading to "capillary stiffness“ resulting into decreased lung`s compliance. The associated congestion increases lung`s viscosity. These two mechanisms intensify the required respiratory work. As for the vicious feedback, elevated PRESP increases LV afterload, while elevated PCT affects the RV afterload. In addition, the left and right atrial V-waves (filling) were significantly and oppositely modulated by respiration. An increase in PRESP in HF patients was associated with more pronounced RA filling and with lower LA filling, possibly contributing to further lung congestion.
Conclusions: The respiratory dynamics and PRESP may be used as a surrogate of the respiratory effort and allow quantification of dyspnea severity. The respiratory effort plays a pivot role in the vicious cycle of cardiac decompensation.
Powered by Eventact EMS