
A Novel Modality for Early Detection of Peripheral Arterial Disease and Assessing the Severity of Atherosclerotic Disease
Introduction: Patients with asymptomatic peripheral arterial disease (PAD) are at high risk of morbidity. Recent guidelines stress the importance of detecting PAD in mitigating the risks of cardiac morbidity and mortality. The guidelines suggest to measure the Ankle-Brachial index (ABI) despite the known limitations of the ABI. We hypothesized that quantification of the peripheral perfusion dynamics can improve the diagnosis.
Methods: A noninvasive technology that continuously monitors extremity perfusion by miniature sensors and impedance electrodes was developed. The perfusion dynamics is analyzed in the time and frequency domains and by wavelet correlations between the legs and various hemodynamic signals. Blood pressure cuffs were placed on the hands and legs to assess the ABI. Partial arterial occlusion was modeled by inflating a blood-pressure cuff around the thigh to 45 and 90 mmHg.
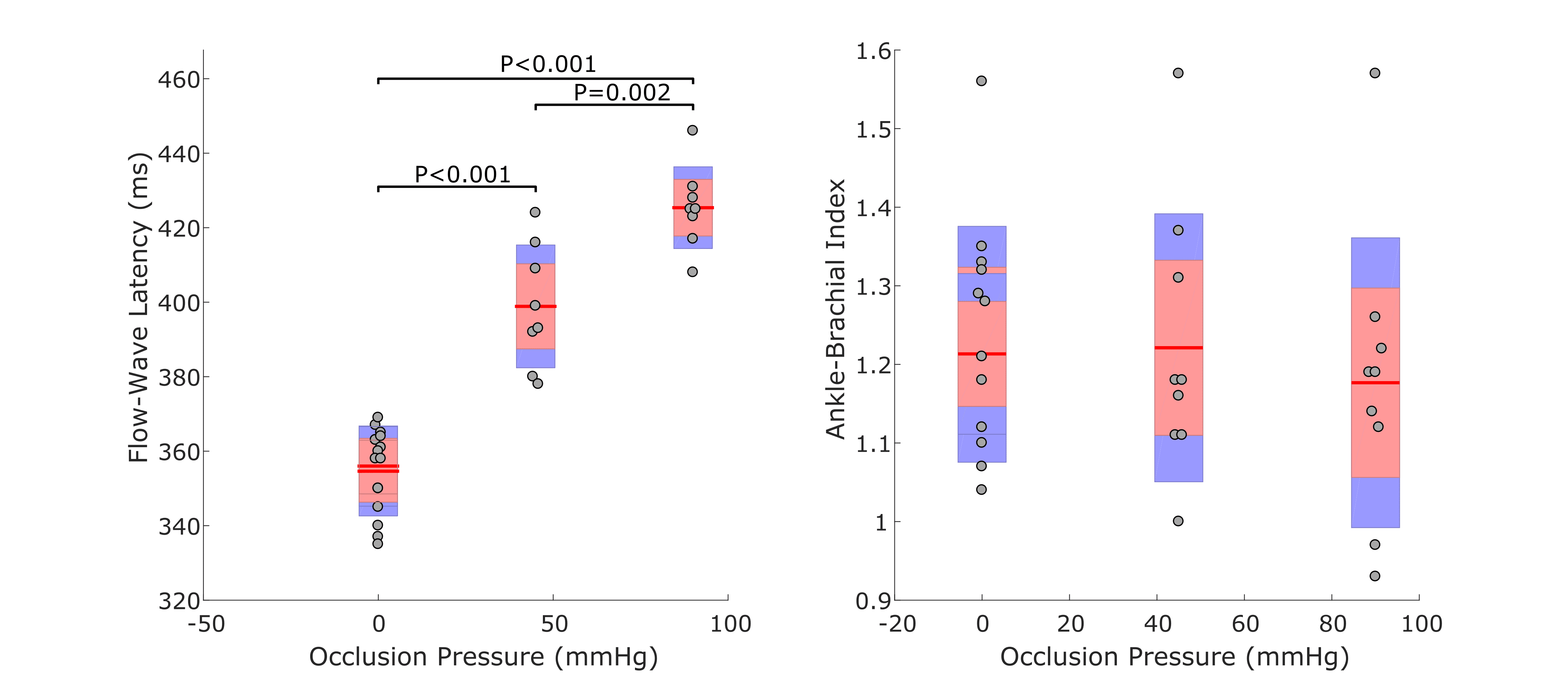
Results: Healthy volunteers (n=8) participated in the study. Partial occlusions yielded pathognomonic measureable indices: flattening of the perfusion dynamics (loss of high frequencies), deceleration of the wave downslopes, and phase delays that were proportional to the degree of the occlusion. Inflating the cuff to 45 and 90 mmHg had no significant effects on the ABI (p>0.54) (Right figure) or the saturation (pulse oximetry). However, it has significant effects on the flow latency, calculated by correlating the perfusion curve with the preceding ECG R-wave (Left figure). The mean flow latency increased from 355±12 to 399±16 (p<0.001) and 425±11 ms (p<0.001) upon application of: zero (baseline), 45 and 90 mmHg of cuff pressure. Partial occlusion of a large artery turns part of the hydrostatic energy into kinetic energy in the narrowed region that returns back into hydrostatic pressure after the obstruction, following a short delay.
Conclusion: Monitoring the perfusion dynamics outperforms the ABI. The utility in early detection of PAD and assessing the severity of atherosclerotic disease require further clinical studies.

Powered by Eventact EMS