Aims: Shifts in populations have drastically increased cardiovascular risk factors and disease rates. We assessed the association between body mass index (BMI) and blood pressure (BP) levels among adolescents of Ethiopian origin and their secular trend of overweight and obesity.
Methods: The study cohort comprised of adolescents aged 16-19 years, who were medically examined prior to military service between 1992 through 2016. Participants of Ethiopian origin were classified into Israeli-born (N=15,793) and immigrants (N=23,487), and adolescents from families that are at least 3 generations in Israel served as controls (n=277,789). BMI was stratified by sex and divided to 6 groups:<17, 17.5-18.4, 18.5-19.9, 20.0-22.4, 22.5-24.9, >25.0 kg/m2. Hypertensive-range BP values adjusted for age, sex and height served as outcome.
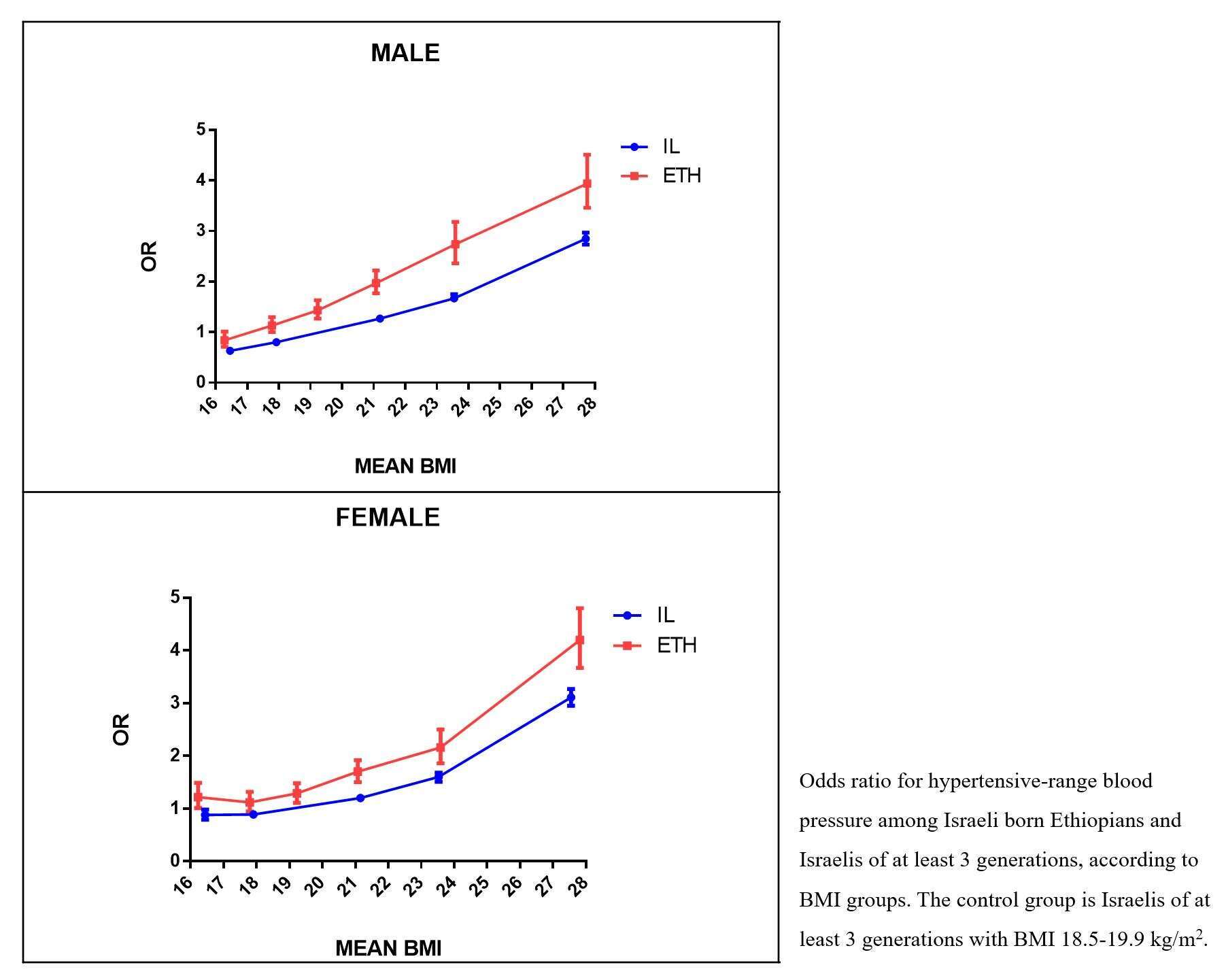
Results: The occurrence of hypertensive-range measurements increased with the length of residency in Israel: 7.3%, 10.6% and 14.4% in males who immigrated at ages 12-19, 6-12 and 0-6 years respectively, and 11.5%, 16.7% and 19.3% among females, respectively. Israeli- born Ethiopians had significantly higher risk for hypertensive range measurements at any given BMI >20 kg/m2 compared to controls, after accounting for socio-demographic variables and medical history. Between 1992 and 2016, there was a 10-fold and 5-fold increase in overweight and obesity in males and females of Ethiopian origin respectively, compared to a 2-fold increase in the controls.
Conclusions: The association between abnormal BP and BMI is significantly steeper among Israelis of Ethiopian origin. This population requires targeted surveillance and appropriate intervention given the dramatic increase in obesity, especially among females.