
Acute Reduction in Neonatal Brain Injury by Selective Blockage of CB1 and Activation of CB2 Receptors
2Department of Biomolecular Sciences, University of Urbino “Carlo Bo”, Italy
Background: Cannabinoids (CBs) can modulate a wide range of neurological and physiological processes through the activation of their receptors, CB1 and CB2. CB receptor agonists and antagonists have demonstrated to produce either protective or toxic responses after brain ischemia. URB447, a CB1 antagonist and CB2 agonist, can selectively block CB1 and activate CB2 receptor signalling.
Objective: Using an in vivo model of neonatal brain injury, to examine the potential therapeutic effect of URB447, given before or after a hypoxic-ischemic (HI) event.
Methods: 7-day-old rat pups received a single intraperitoneal injection of URB447, i) 1 hour before starting the ischemic procedure (HI+URB447 1h-PRE), ii) 30 minutes (HI+URB447 30min-POST) or iii) 3 hours (HI+URB447 3h-POST) after hypoxia. To test if the protective effect of URB447 was mediated by CB1/CB2 modulation, WIN-55212, a CB1/CB2 receptor agonist, was injected i.p. 1h and 30 minutes before HI (HI+WIN-55212) or 30 minutes before URB447 administration (HI+URB447+WIN-55212). Each HI-injured group (HI) received a corresponding volume of vehicle. N=10 for all groups. The neuroprotective effect of drugs was assessed using histological and molecular techniques in 14 day-old animals.
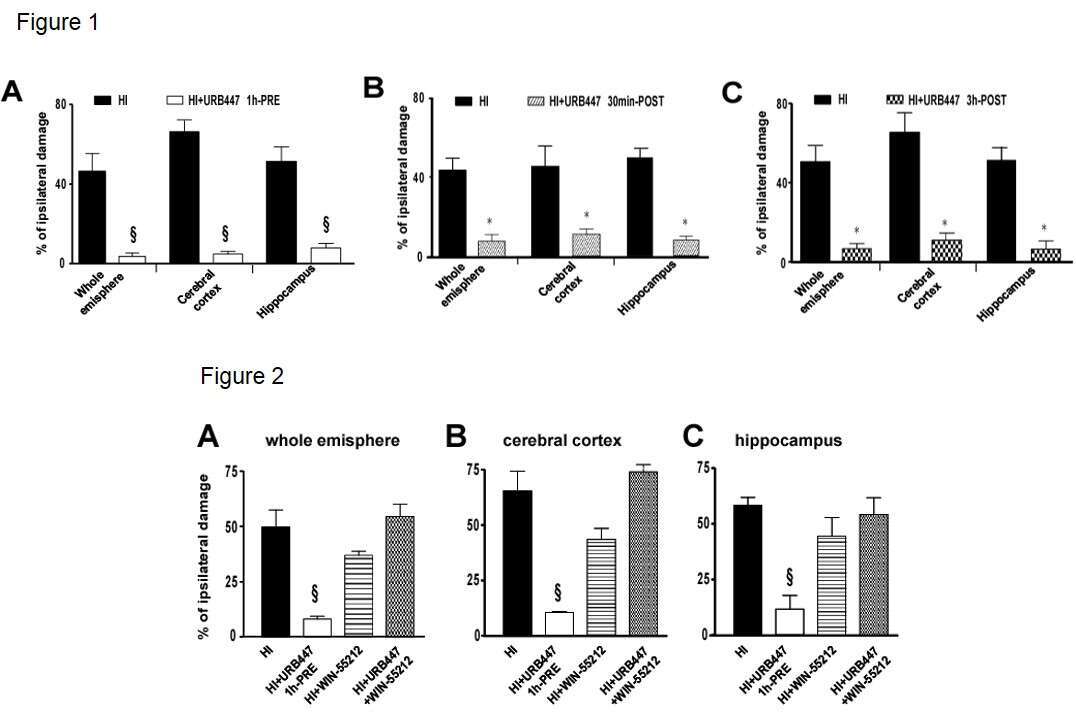
Results: HI-induced reduction in whole hemisphere (46.5%) and cerebral cortex (65.7%) areas was avoided after URB447 administration, showing a decrease in brain infarction both before (whole hemisphere: 83.7%; cerebral cortex: 92.7%) and 30 min after (whole hemisphere: 95.7%; cerebral cortex: 95.4%) the injury (Fig.1). WIN-55212 completely blocked the neuroprotective effect of URB447 (Fig.2). Of clinical relevance, URB447 injected 3 hours after HI reduced brain infarction 95.7% and 88% in whole hemisphere and cerebral cortex, respectively (Fig.1). Furthermore, delayed cell death, astrogliosis and white matter damage returned to those values observed in sham animals.
Conclusion: Selective blockage of CB1 and activation of CB2 receptors induce an acute reduction in brain injury in the neonatal rat. Grants: UPV/EHU (GAITUZ2019, GIU17/018).
Powered by Eventact EMS