
Changes Over Time in Serum Albumin Levels Predict Outcomes following Percutaneous Coronary Intervention
Background: Evidence is growing, identifying serum albumin levels as a powerful prognostic marker in the full spectrum of cardiovascular diseases, even after adjusting for traditional risk factors and potential confounders
Objectives: To evaluate the prognostic significance of changes in serum albumin levels among patients that underwent percutaneous coronary intervention (PCI).
Methods: Patients who underwent PCI in a tertiary medical center throughout 2004-2016 were considered for the study. Patients with missing serum albumin levels within the year before or after the PCI were excluded from the study as well as those for whom serum albumin levels were obtained throughout an acute infection. Changes in albumin were represented by ∆albumin: Albumin before PCI (closest) minus lowest albumin within the year following the PCI. ∆albumin was categorized by the median and into quartiles (Q1-Q4). The outcomes were all-cause mortality or major adverse cardiac events (MACE).
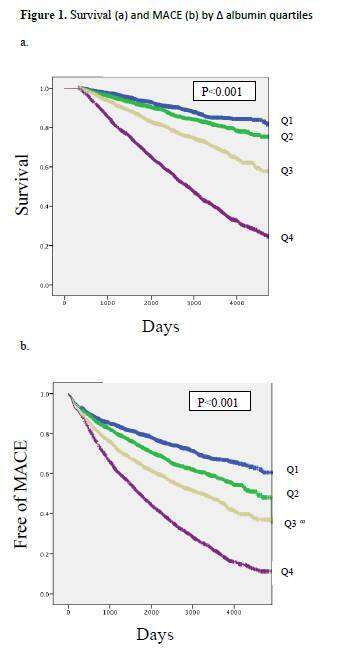
Results: The study included a total of 7,511 patients, mean age 65.8 ±12 years, 23% women. The median ∆albumin was 0.5 g/dL. Patients with above median ∆albumin were older with higher prevalence of most cardiovascular risk factors, CHF, CABG, baseline creatinine, malignancies and baseline albumin compared with patients with below median ∆albumin. The follow-up period was 8.1 years (median), with cumulative all-cause mortality rate 27% and the MACE rate 46%. Mortality and MACE rates (figure 1) increased gradually as the ∆albumin quartile increases Q1 (10%, 26%), Q2 (14%, 35%), Q3 (25%, 47%), Q4 (56%, 74%), respectively, (p
Conclusions: ∆albumin is an independent and incremental long-term prognostic marker following PCI, beyond that of baseline serum albumin levels. Routine follow-up of serum albumin levels in these patients should be considered.

Powered by Eventact EMS