
Clinical Features and Outcomes of Coronary Revascularization in Very-old Patients with Left Main Disease
Background: Coronary artery disease (CAD) is often more extensive and calcified in older adults, and may involve multivessel and left-main coronary artery (LMCA) disease. Elderly patients are commonly excluded from clinical trials and limited real-world data exist on the management and outcomes of significant LMCA disease in the very-old.
Objectives: To investigate clinical features and outcomes of very-old patients undergoing revascularization by percutaneous coronary intervention (PCI) or coronary artery bypass surgery (CABG), due to LMCA disease.
Methods: Retrospective single center analysis of patients ≥80 years (n=139) who underwent revascularization due to CAD involving unprotected LMCA stenosis >50%. Subsequent major adverse cardiovascular events (MACE: myocardial infarction, stroke and all-cause death) and repeat revascularizations were recorded, and their relation to revascularization procedure was studied.
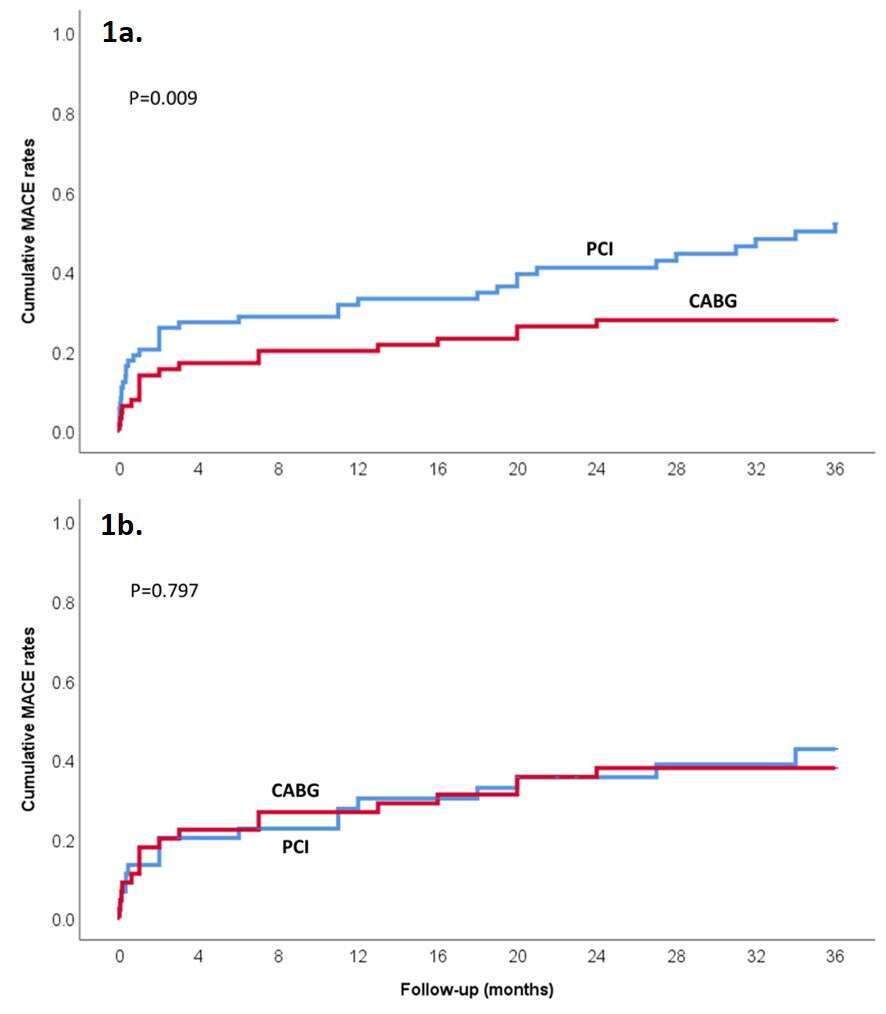
Results: PCI was performed in 74 patients and CABG in 65. Most patients (80%) had multivessel disease involving ≥2 additional coronary arteries. PCI was associated with older age and higher rates of baseline disability, previous revascularization, reduced ventricular function, significant aortic stenosis and presentation with acute coronary syndrome, compared to CABG. Cumulative 3-year MACE rates were higher in patients undergoing PCI versus CABG (p=0.009; Figure-1a). After multivariable adjustment, predictors of MACE included presentation with acute STEMI [HR=2.39, 95%CI 1.24-4.63, p=0.010], revascularization by PCI compared to CABG [HR=2.21 (1.18-4.15), p=0.013], baseline disability [HR=2.17 (1.20-3.91), p=0.010] and distal/bifurcation LMCA disease [HR=1.87 (1.04-3.38), p=0.038]. The difference in 3-year MACE between PCI and CABG was not observed in a propensity-score analysis of 90 patients matched 1:1 for baseline disability, STEMI and aortic stenosis (p=0.797; Figure-1b).
Conclusions: In very-old patients undergoing coronary revascularization due to LMCA disease, PCI was associated with worse cardiovascular outcomes compared to CABG, influenced by a more severe and comorbid population selected for PCI. Baseline disability, presentation with STEMI and distal LMCA bifurcation disease, were additional independent outcome predictors.

Powered by Eventact EMS