
Stopping at a Community Clinic and Self-evacuation Substantially Delays Emergency Department Arrival in Patients Presenting with an Acute ST-Elevation Myocardial Infarction
2The Azrieli Faculty of Medicine, Bar Ilan University
Background: Longer ischemia time is known to be related to adverse outcomes in patients with acute ST elevation myocardial infarction (STEMI). Shortening the time from emergency department (ED) to reperfusion has been largely addressed could be rather easily controlled. Time from symptoms onset to ED has been less studied. The aim of this study was to define the clinical, residential and transportation associates of longer pre hospital delay in STEMI.
Methods: Patients presenting to our facility with STEMI between 2-2015 and 12-2017 were retrospectively identified (n=308). Excluding inpatients, missing time of pain onset and cardiac arrest left 266 patients for analysis. Clinical and transport data were retrieved from the cardiology department database. Analysis was done by ANOVA and multivariable logistic regression.
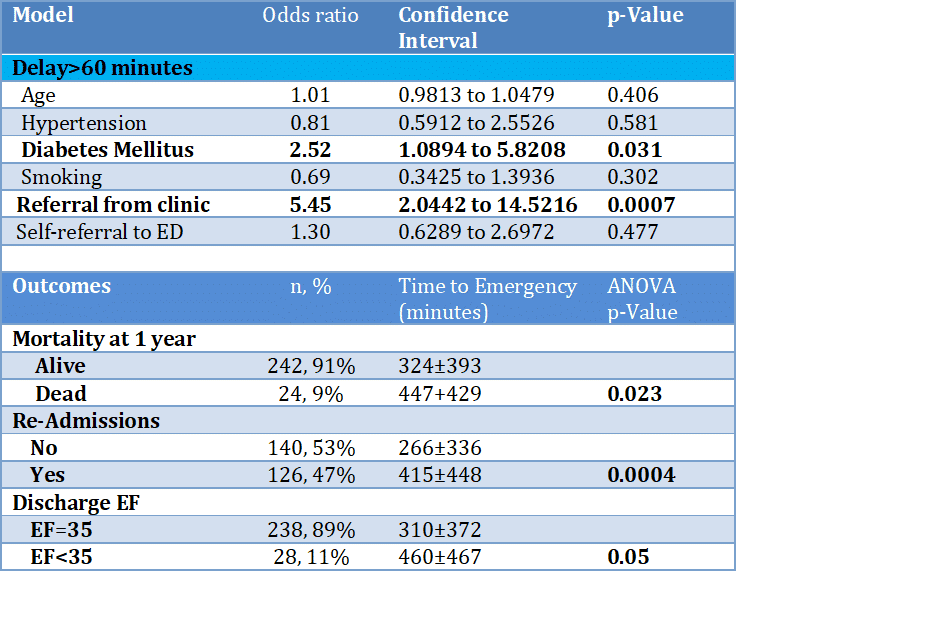
Results: Patients were 61±11 years old (81% male), living 21±12km form our hospital. Univariate associates of longer delay included diabetes mellitus, hypertension, non-smoking, self-evacuation to ED and referral from a community clinic. On multivariable logistic regression analysis (table) a stop at the community clinic was associated with a >5 times risk of a longer than an hour delay, and diabetes more than doubled it. Longer delays were associated with discharge ejection fraction <35%, readmissions and 1 year mortality (Table). Evacuation from clinic by ambulance halved the time to ED compared to self-evacuation (367±46 vs.736±55minutes, p<0.0001, respectively).
Conclusion: The strongest determinant of pre-hospital delay in STEMI was stopping at a community clinic first. Longer pre-hospital delays was translated into worse outcomes. This suggests that people, especially those with risk factors should be educated regarding the presentation of STEMI and that they should seek medical help via an ambulance where the diagnosis and initial medical treatment are done in transit on the way to the ED. Community clinics should probably be instructed to complete the journey to the ED by ambulance.
Powered by Eventact EMS