
The Charlson Comorbidity Index: A Significant Predictor of Increased Mortality and Cardiac-Related Hospitalizations in Patients with Heart Failure
Background: Comorbidities are highly prevalent in patients with heart failure (HF) and are suggested to have an impact on clinical outcome. The Charlson comorbidity index is a validated score to estimate mortality in patients with multiple comorbidities. We evaluated the predictive value of this score on clinical outcome in patients with HF.
Methods: All patients with a diagnosis of chronic HF and the Charlson comorbidity index at a health maintenance organization were evaluated. Patients were followed for cardiac-related hospitalizations and death.
Results: The cohort included 6,404 HF patients. Mean follow-up was 576 days; the median Charlson score was 6 (interquartile range 5-7); age-adjusted Charlson score was 9 (8-10). The Charlson score and the age-adjusted Charlson score were discriminative and significant predictors of survival as well predictive of the combined endpoint of death and cardiovascular hospitalization (Figure 1). After adjustment for other significant predictors, increasing Charlson score and age-adjusted Charlson score were independently predictive of survival and the combined endpoint of death and cardiovascular hospitalization by Cox regression analysis. The area under the curve (AUC) by receiver operating curve (ROC) for the Charlson, age-adjusted Charlson and the HF adjusted model were 0.62; 0.65 and 0.715 respectively (P
Conclusions: Comorbidities as evident by the Charlson comorbidity index have a significant impact on outcome in HF patients.
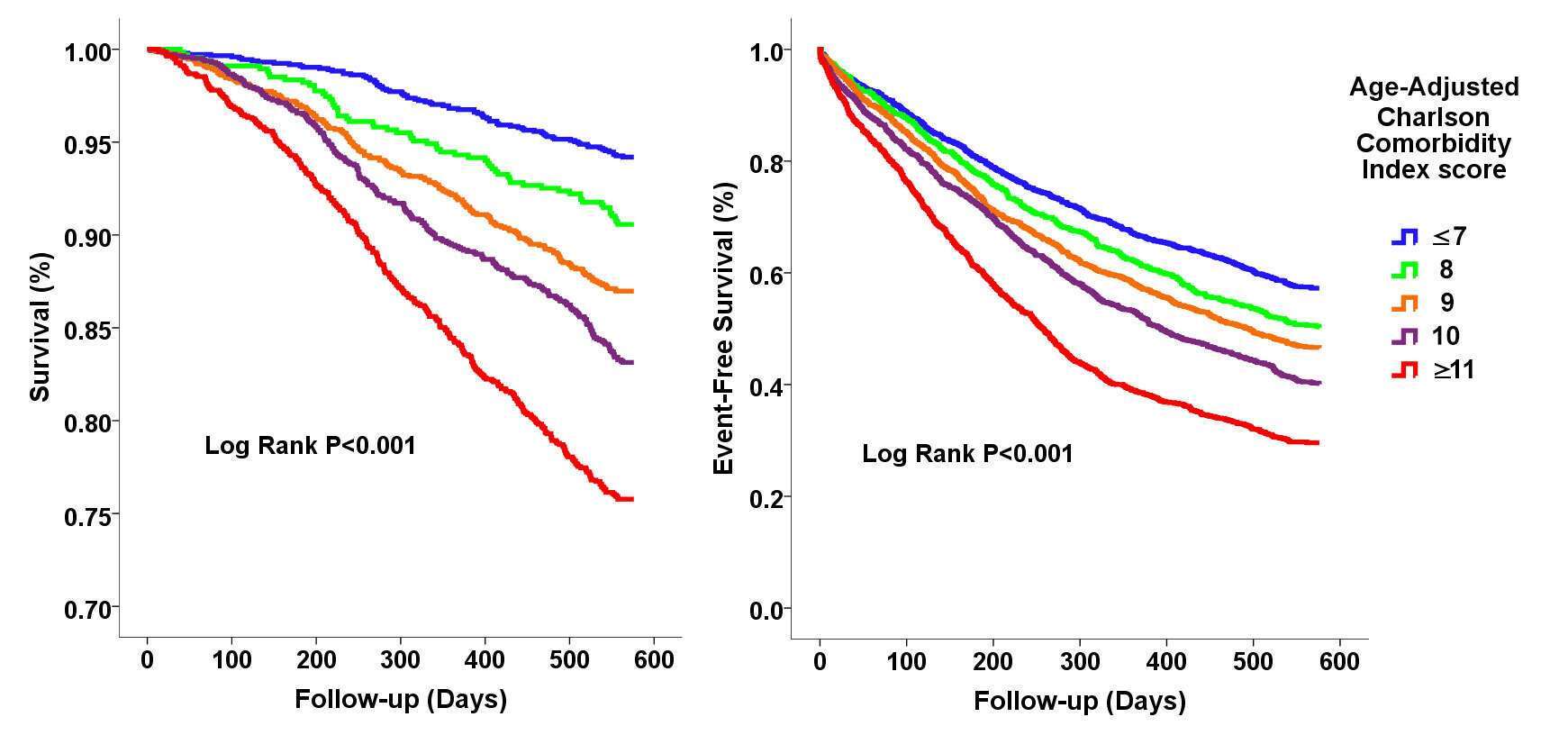
Figure 1. Survival and event-free survival from death and cardiovascular hospitalization by Kaplan-Meier survival analysis stratified by quintiles of age-adjusted Charlson comorbidity index.

Powered by Eventact EMS