
Gender Disparities in Non-ST Elevation Myocardial Infarction Management and Outcome: Insight from Sheba Big Data
Background: Women are underrepresented in randomized clinical trial. The purpose of the current study was to evaluate gender disparities in management and outcome of patient with non-ST segment myocardial infarction (NSTEMI) in contemporary real-world settings in Israel.
Methods: Data source for the current analysis was Sheba Medical Center electronic health records. All consecutive patients who were hospitalized in internal medicine or cardiology departments with NSTEMI as clinical diagnosis between 06/2011 and 10/2018 were included.
Results: Final study cohort included 5,559 patients with a median follow up of 2 (IQR 1-4) years. Mean age of the study population was 72 ± 14 years and 1,764 (32%) were women. Compared with men, women were older (77±12 vs. 69±14, p<.001), had lower levels of troponin (2.8±7.1 vs. 3.5, p=.003) and Haemoglobin (11.6±1.9 vs. 12.9±2.3, p<.001). Women were significantly less likely to be hospitalized in the cardiology department (27% vs. 47%, p<.001) and had a slightly longer hospital stay (5.3±4.5 days vs. 5.0±5.3, p=.04). With respect to clinical management, women were less likely to undergo coronary angiogram during hospital say (42% vs. 63%, p<.001). Sub-analysis of all 3,114 (56%) patient who underwent in-hospital coronary angiogram demonstrated that women were less likely to undergo percutaneous coronary intervention (58% vs. 70%, p<.001). Kaplan Meier survival analysis demonstrated worse overall survival among women (p<.001;FIGURE). However, multivariate cox regression with adjustment to known predictors of poor outcome including hospitalization department and invasive approach showed that women were 21% more less to die during follow up(95% CI .71-.88,p=<.001).
Conclusion: In this contemporary cohort, women with NSTEMI are older , less likely to be admitted to the cardiology department, and less likely to undergo a coronary angiogram or intervention. However, after adjustment to other predictors of poor outcome, women with NSTEMI have better overall survival compared with man.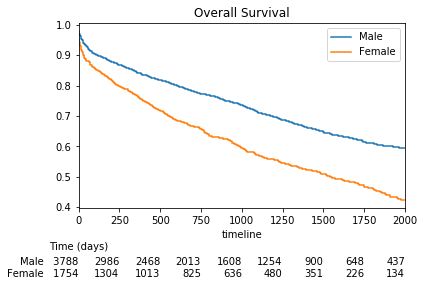
Powered by Eventact EMS