
Coronary Arterial Lesions and Intravenous Immunoglobulin Resistance in Kawasaki Disease: A Case-Control Study
2Department of General Paediatrics and Paediatric Infectious Diseases, Hospital Universitario La Paz, Spain
3Department of Paediatric Cardiology, Hospital Universitario La Paz, Spain
4Paediatric Emergency Department, Hospital Universitario La Paz, Spain
5Department of Paediatric Radiology, Hospital Universitario La Paz, Spain
6Paediatric Intensive Care Unit, Hospital Universitario La Paz, Spain
7Department of Paediatric Reumatology, Hospital Universitario La Paz, Spain
Backgroung: The most important complication related to Kawasaki Disease (KD) are coronary arterial lesions, mainly aneurisms. Although several drugs have been used for this disease, the only treatment that decreases coronary lesions is intravenous immunoglobulin (IVIG). However, fever persists or reappears in 20% of the patients with KD treated with IVIG, which is called IGIV resistance. IGIV resistance has been linked to an increased risk of coronary damage.
Objective: The aim of this study was to compare the frequency and the severity of coronary arterial lesions among resistant and responsive KD patients treated with IVIG in a Spanish tertiary hospital.
Methods: We performed a case-control study. It included 38 KD patients who were resistant to IVIG (cases) in a period of 16 years. We chose 2 IVIG responsive KD patients (controls) per each case, the immediately previous and after ones.
Results: The incidence of resistance to IVIG in our KD patients was 18%.
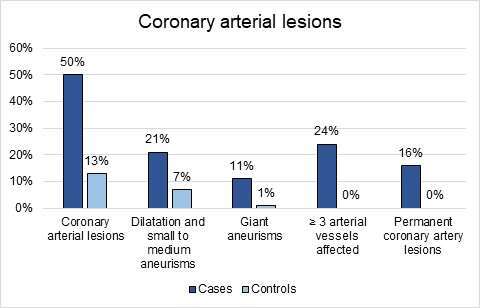
Coronary damage was present in 50% of our resistant patients, whilst its incidence in responsive patients was 13%. Furthermore, resistant patients suffered severe coronary arterial lesions more frequently compared to responsive patients (11% vs 1%). Not only severe lesions were more usual, but also the mild ones (21% vs 7%).
The extension of injury was higher in resistant patients. 24% of the unresponsive patients showed 3 or more vessels affected, while none of the responsive patients had such extensive damage.
Moreover, all the coronary arterial lesions were transient in patients with good response, but in 16% of the unresponsive patients, lesions were permanent.
Conclusion: Resistance to IVIG is quite common in our KD patients. It is related to higher risk, severity, extension and duration of coronary damage. Thus, prediction, early detection and close follow-up are necessary to adequate the treatment and improve the prognosis of these patients.
Powered by Eventact EMS