
Fatal Streptococcus pneumoniae Meningoencephalitis in a Fully Vaccinated 4 Year Old Boy
2Department of Radiology, Mater Dei Hospital, Malta
A previously healthy four year old boy, born to non-consanguineous parents, had minor coryzal symptoms, fever and vomiting for 36 hours, treated empirically with oral antibiotics by GP. He was found jerking and unresponsive and rushed to hospital with a temperature of 37.8OC and status epilepticus refractory to mannitol and repeated doses of midazolam and phenytoin. Shortly after admission, his conscious level deteriorated, requiring intubation and transfer to Intensive Care.
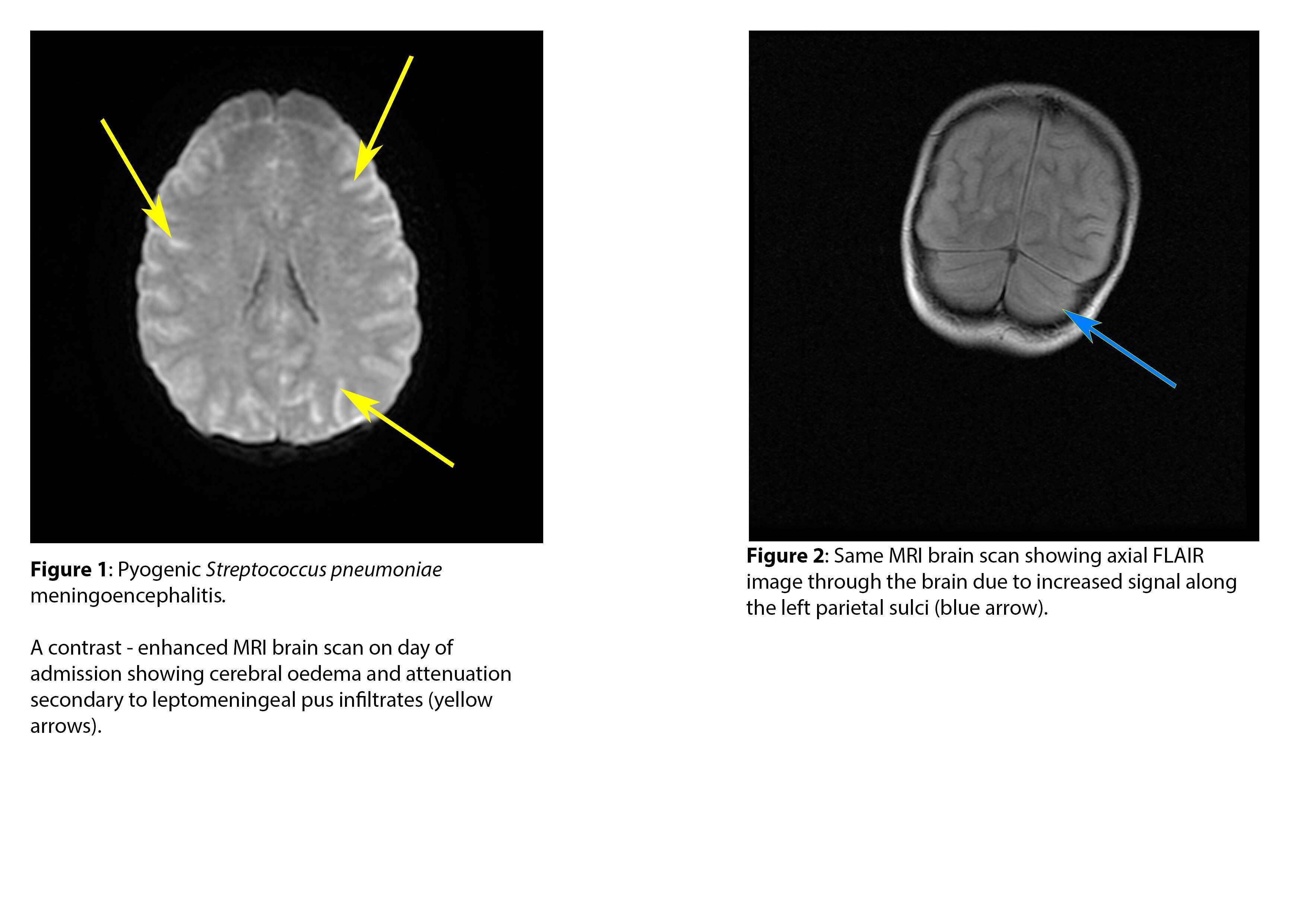
The white cell count was 44x109 cells/L, with a neutrophilia of 41.31x109cells/L. His CRP was 233mg/L on admission and 627mg/L after 2 days. A CT and MRI brain scans done within hours of admission revealed meningoencephalitis with widespread meningeal pus-infiltrates, cerebral swelling, impaired diffusion, raised intracranial pressure and brainstem herniation ( Refer to Figure1 and 2). The intracranial bolt pressure was 91mmHg. Serum was PCR positive for Streptococcus pneumoniae, later confirmed as capsulated serotype 19F. He received ceftriaxone, vancomycin, metronidazole, clarithromycin and acyclovir without clinical improvement.Repeated brainstem function was absent after 3 days and life support was discontinued.
He had received all childhood vaccinations including four doses of a pneumococcal conjugate vaccine. There was no asplenia however immunoglobulins were low: IgG <1.2g/L (5.46-17.6), IgM 0.13g/L (0.26-1.21), and IgA 0.23g/L (0.52-2.84). Despite MMR and hepatitis B vaccination, he tested negative for Rubella and Hepatitis B surface IgG antibodies. A diagnosis of agammaglobulinaemia, possibly X-linked (XLA), was considered, particularly since a maternal first cousin had died of severe sepsis in childhood. In fact, subsequent DNA studies showed X-linked agammaglobulinaemia:c.871G>C hemizygote in BTK gene. Maternal DNA is still being investigated.
The primary antibody deficiency syndromes, including XLA, usually present with recurrent respiratory tract infections due to an inability to mount an effective immunoglobulin response. Limited awareness of the presenting features commonly gives rise to diagnostic delays or fulminant septicaemia. Therapy consists of Ig replacement therapy and prophylactic antibiotics with resultant increased life expectancy by reducing the frequency and severity of infections. Earlier diagnosis with neonatal screening for those with a family history is the current ‘best option’, whilst bone marrow transplant and gene therapy offer a potential cure in these patients.
Powered by Eventact EMS