
Intermittent Irritability in a Toddler
2Paediatrics - Infecciology Unit, Centro Hospitalar Lisboa Norte - Hospital Santa Maria - Centro académico de Lisboa, Portugal
3Orthopedic Unit, Centro Hospitalar Lisboa Norte - Hospital Santa Maria - Centro académico de Lisboa, Portugal
Background/Objective: Spondylodiscitis is a rare entity in pediatrics. The low specificity of symptoms and laboratory data, the scarcity of physical examination findings and the late radiographic changes justify the usually late diagnosis.
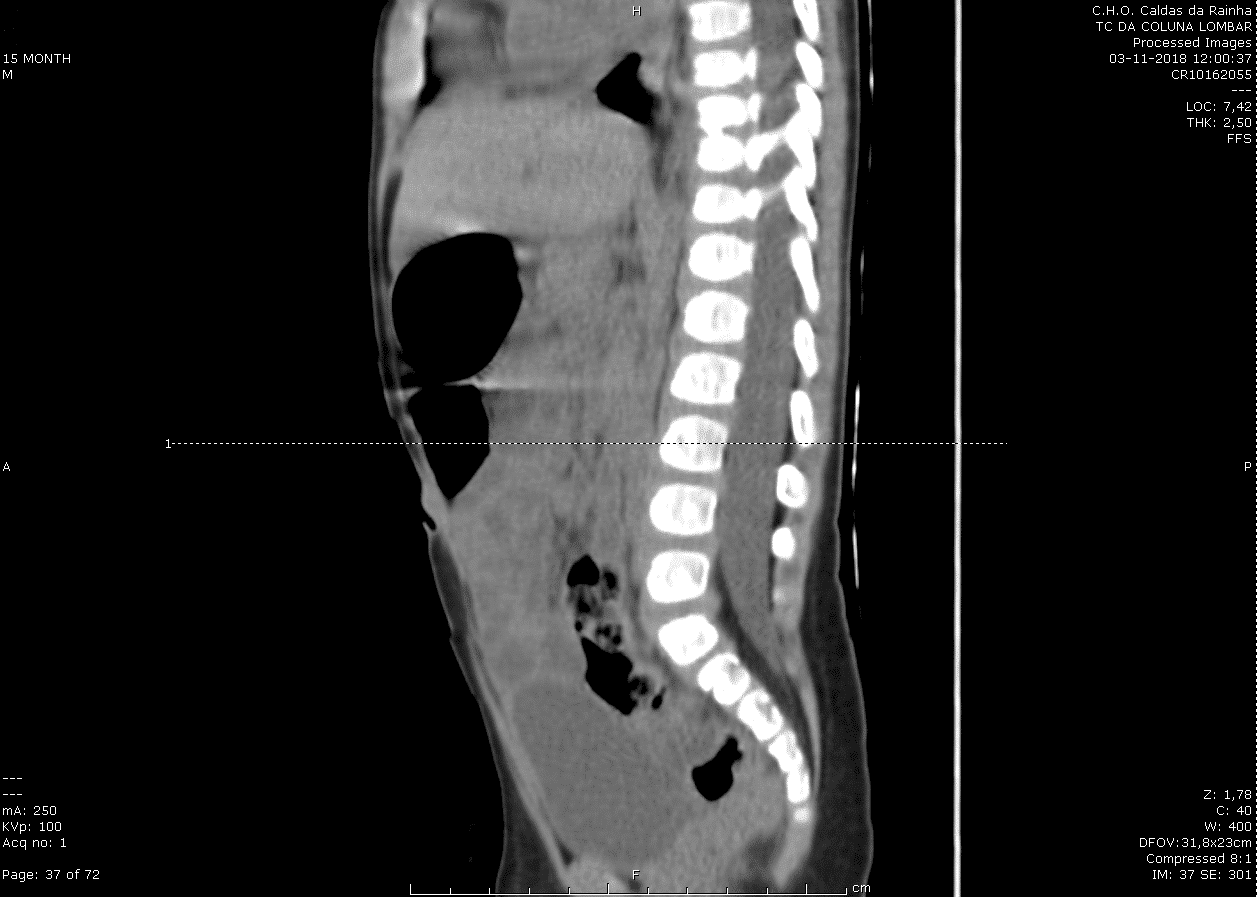
Methods: 15-month-old boy with irrelevant personal and family history. Presented to our emergency department with notion of pain in the previous 15 days, characterized by periods of polypnea and irritability. Progressive worsening in the previous week, with nocturnal awakening, improvement with ibuprofen, and antalgic position in dorsal decubitus or lumbar hyperextension, with gait refusal in the last days. History of diarrhea 2 weeks before admission. He looked prostrate, complaining while sitting but had no pain in passive mobilization of the lower limbs or in palpation/percussion of the spine. He started fever at the hospital that persisted for 2 days. The blood panel showed ESR 55mm and ALP 1076 U/L and no increase in CRP or leukocytosis. CT showed vertebral irregularity of D9-D10 with possible relation to bone destruction secondary to spondylodiscitis.
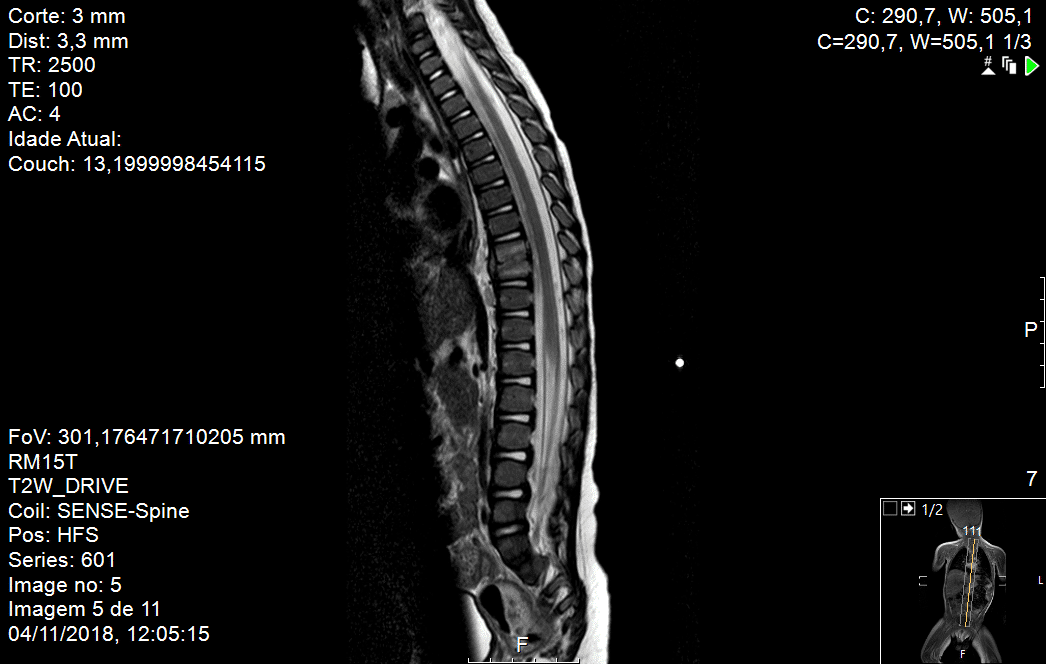
He was transferred to a tertiary hospital, where the MRI confirmed the diagnosis.
Serologies for Brucella, Bartonella and Coxiella, blood culture, IGRA and PCR for bacterial DNA were negative. After 8 days of intravenous ceftriaxone IV he was asymptomatic and was discharged with oral amoxicillin and clavulanic acid for 5 weeks.
Conclusion: Spondylodiscitis usually has an insidious onset of symptoms. Although children may report low back and walking pain, infants may initially only show nonspecific signs such as irritability. Therefore, it is important to remember this illness, especially as it may have serious complications. MRI is the key standard for an early diagnosis and follow-up of disease progression.
Powered by Eventact EMS