
Infantile Hemangioma
2Serviço de Dermatologia, Centro Hospitalar do Porto, Portugal
3Serviço de Neonatologia, Hospital Pedro Hispano, Portugal
Background: Infantile hemangiomas (IHs) are skin lesions characterized by abnormal proliferation of endotelial cells and aberrant blood vessel architecture. They represent the most common tumors in childhood, affecting 5% of general population. Risk factors include low birth weight, caucasian race or female gender. In most cases, IHs are diagnosed based on disease history and physical exam. Manifestations are usually present before 4 weeks of age and growth is completed by 5 – 8 months of age (proliferative phase). Then it starts to involute until it disappears, frequently by the age of 4 years (involution phase). It might occur ulceration and pain, and due to localization on or near vital structures may cause functional impairment or permanent disfigurement. Imaging is not usually necessary, but when performed, ultrasound is generally the preferred modality for diagnosis, whereas magnetic resonance imaging (MRI) is requested to assess the extent of lesion. Although the majority of IH’s resolves spontaneously, ulcerated IHs or near vital structures require early consultation with a dermatologist.
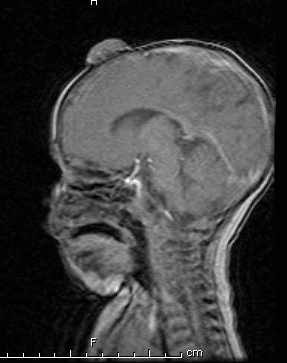
Case Report: A one-month-old infant, born at 37 +5 weeks and weighted 2540g, was examined for a progressively increasing right frontoparietal infantile hemangioma. The ultrasound was compatible with the clinical diagnosis of a 3.2 cm hemangioma reaching the anterior bording of the anterior fontanelle. The MRI confirmed the bone involvement. The patient was referred to Dermatology and started propranolol 2 mg/kg/day tid. Baseline electrocardiogram and echocardiogram were normal. Monitoring was performed by a pediatric cardiologist. IH significantly reduced after 6 months of therapy, without complications.
Conclusion: Although most IHs do not require treatment, a minority may develop severe complications, requiring therapeutic intervention. Imaging may be needed when evaluation of extent is necessary. Pediatric providers should remain watchful. When justified, propranolol administered orally at a dose of 2 mg/kg per day is efficacious in reducing IHs.

Powered by Eventact EMS