
Intracerebral Hemorrhage in an Eight Year Old Girl
2Department of Pediatrics, Faculty of Medical Sciences - University "Goce Delcev" Stip, Macedonia
Background: Intracerebral hemorrhage (ICH) rarely occurs in children. The most common underlying cause for ICH in the pediatric population are arteriovenous malformations, cavernous malformations and aneurysms. The rate of ICH among children is reported to be 0.8/100,000 person-years resulting in mortality up to 33% and major deficits up to 40%, including seizures, cognitive and motor impairments.
Objective: To present a pediatric case of spontaneous ICH as a result of cerebral vascular malformation.
Methods: Eight year old girl presented with acute onset headache, abdominal pain, nausea, vomiting and hand crumps. On physical examination conscious, afebrile, pale, dehydrated. Blood tests, examinations by ophthalmologist, otorhinolaryngologist and a general surgeon, combined with abdominal ultrasound examination, all with no pathological evidence. Non-contrast computed tomography (CT) scan demonstrated an oval hyperdensed mass with dimensions 27 x 19 mm, on the right temporo-occipital region, subcortically with a local edema and calcifications. CT angiography (CTA), MRI and MRI angiography demonstrated a lesion corresponding to disrupted cavernous angiomas with a possible transformation into venous angiomas and compressive effect of trigonum on the right lateral ventricle. Patient was observed by neurosurgeon and treated symptomatically.
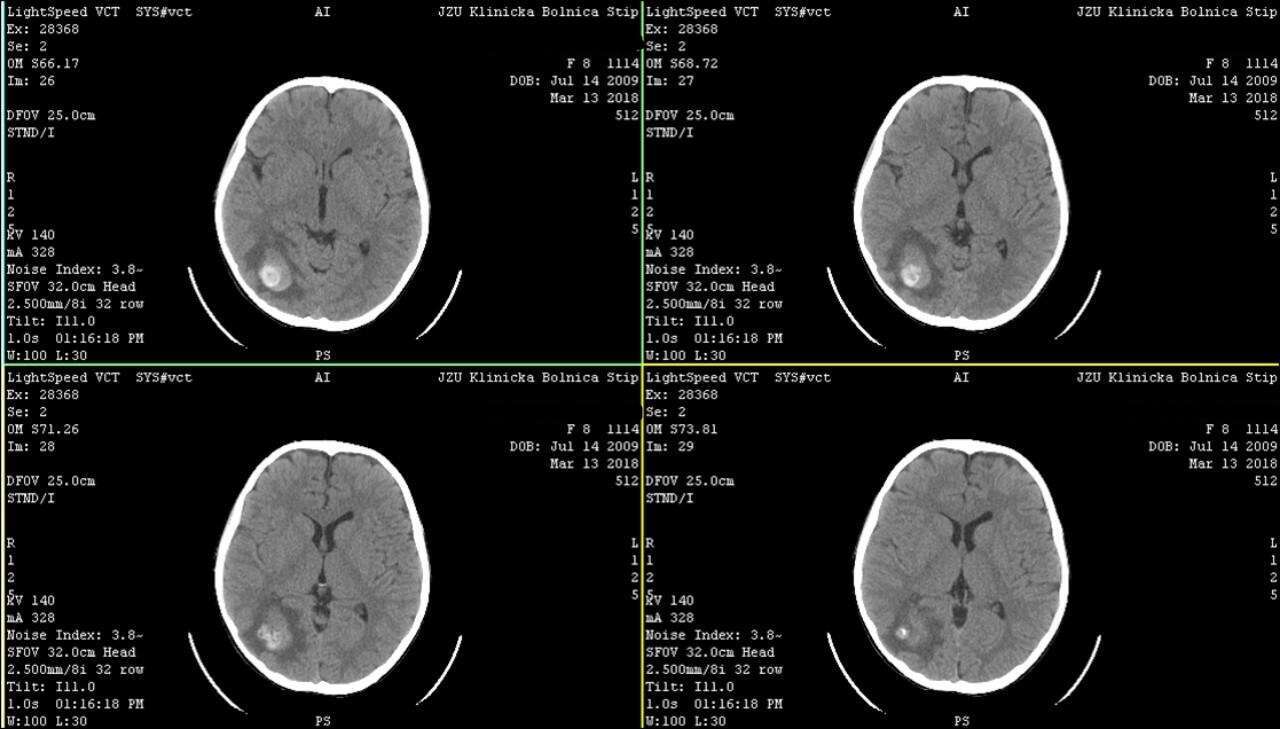
Non-contrast CT
Results: Two days after hospital discharge with epileptic seizure treated outpatient with antiepileptic drugs (Carbamazepin) and Vitamin C. Control MRI demonstrated complete resorption of bleeding with the presence of a small cavernoma in the parieto-occipital right region. Six months after initial ICH, cavernoma was surgically removed. Control MRI of brain in favor of complete excision of the cavernoma. Postoperative without epileptic seizures but still on antiepileptics and Vitamin C.
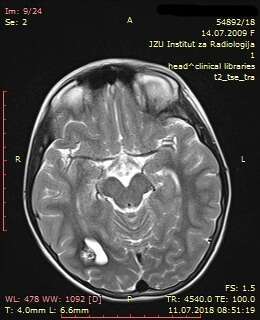
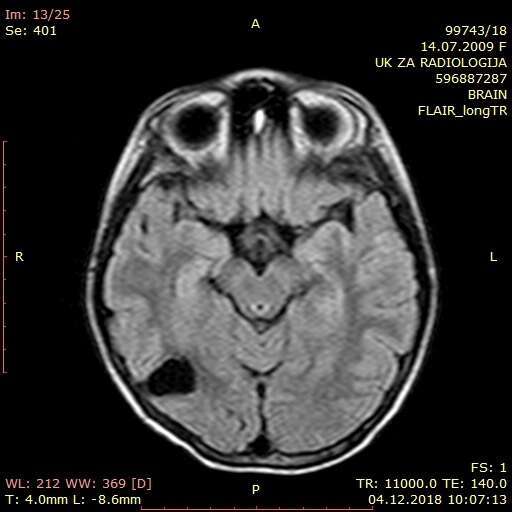
Preoperative MRI and Postoperative MRI
Conclusion: Rupture of brain vascular malformations can cause intracerebral or subarachnoid bleeding. The pressure to the surrounding brain structures, necrosis and focal changes, can develop neurological signs and epileptic seizures as in this case.
Powered by Eventact EMS