
Outcomes of Critical Congenital Heart Disease in Premature Infants at a Single Referral Centre
2Department of Pediatrics, Soonchunhyang University Hospital, South Korea
3Department of Pediatrics, Jeju National University Hospital, South Korea
4Department of Pediatrics, Seoul National University, South Korea
6Department of Thoracic and Cardiovascular Surgery, Seoul National University, South Korea
Background: Despite advances in neonatal intensive care and surgical procedures, perinatal mortality rates for premature neonates with congenital heart disease (CHD) are relatively high, and survivors are at risk for short-term morbidity and adverse neurological outcomes.
Objective: We aimed to describe the outcomes of premature neonates with critical CHD and to identify the risk factors associated with in-hospital mortality at a single referral tertiary centre.
Methods: This was a retrospective cohort study of premature neonates with critical CHD admitted to the neonatal intensive care unit from January 2005 to December 2016.
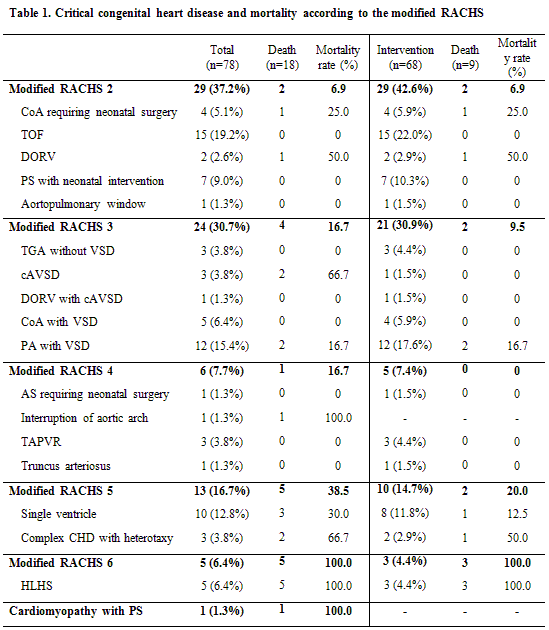
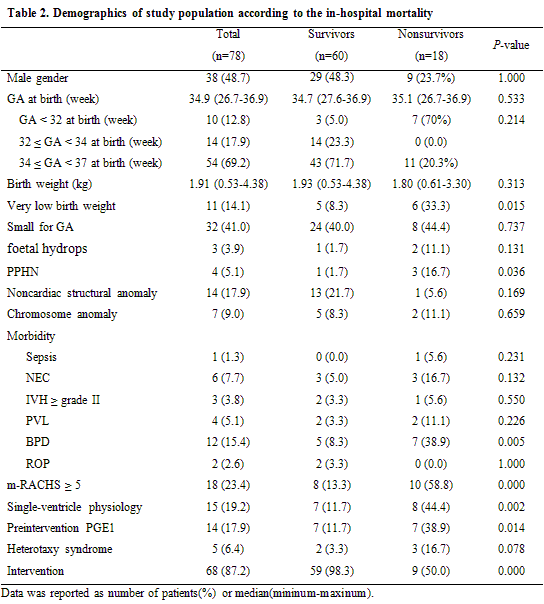
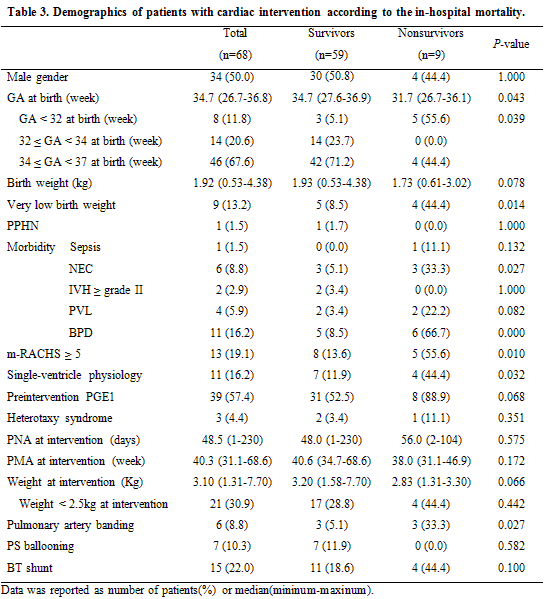
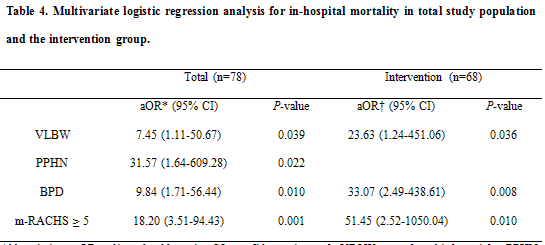
Results: A total of 78 premature neonates were enrolled (male 38, 48.7%). The median gestational age (GA) at birth was 34.9 (26.7-36.9) weeks, and the median birth weight was 1.91 (0.53-4.38) kg. A surgical or percutaneous intervention was performed in 68 patients with a median GA at birth of 34.7 (26.7-36.8) weeks and a median birth weight of 1.92 (0.53-4.38) kg. The in-hospital survival rate was 76.9% among all enrolled preterm infants and 86.8% among patients who received an intervention. Very low birth weight (VLBW), persistent pulmonary hypertension of the newborn (PPHN), bronchopulmonary dysplasia (BPD), and CHD complexity were independently associated with in-hospital mortality. For the 68 premature neonates undergoing cardiac interventions, independent risk factors for mortality were VLBW, BPD, and CHD complexity.
Conclusion: For premature neonates with critical CHD, VLBW, PPHN, BPD, and CHD complexity were risk factors for mortality. Careful approaches for surgical intervention and prenatal care should be guaranteed according to the type of CHD and neonatal conditions.
Powered by Eventact EMS