
Hemodynamic Impact of Early Extubation in Children after Cardiac Surgery
Background: Pulmonary hypertension is associated with high morbidity and mortality after pediatric cardiac surgery, perceived as a contraindication for early extubation. This has been a common goal since the 1980’s and today is a regular part of the postoperative protocols. Little is known about the impact of early extubation on pulmonary arterial hypertension after surgery.
Objective: Evaluate the hemodynamic impact of early extubation in children with varying degrees of pulmonary arterial hypertension.
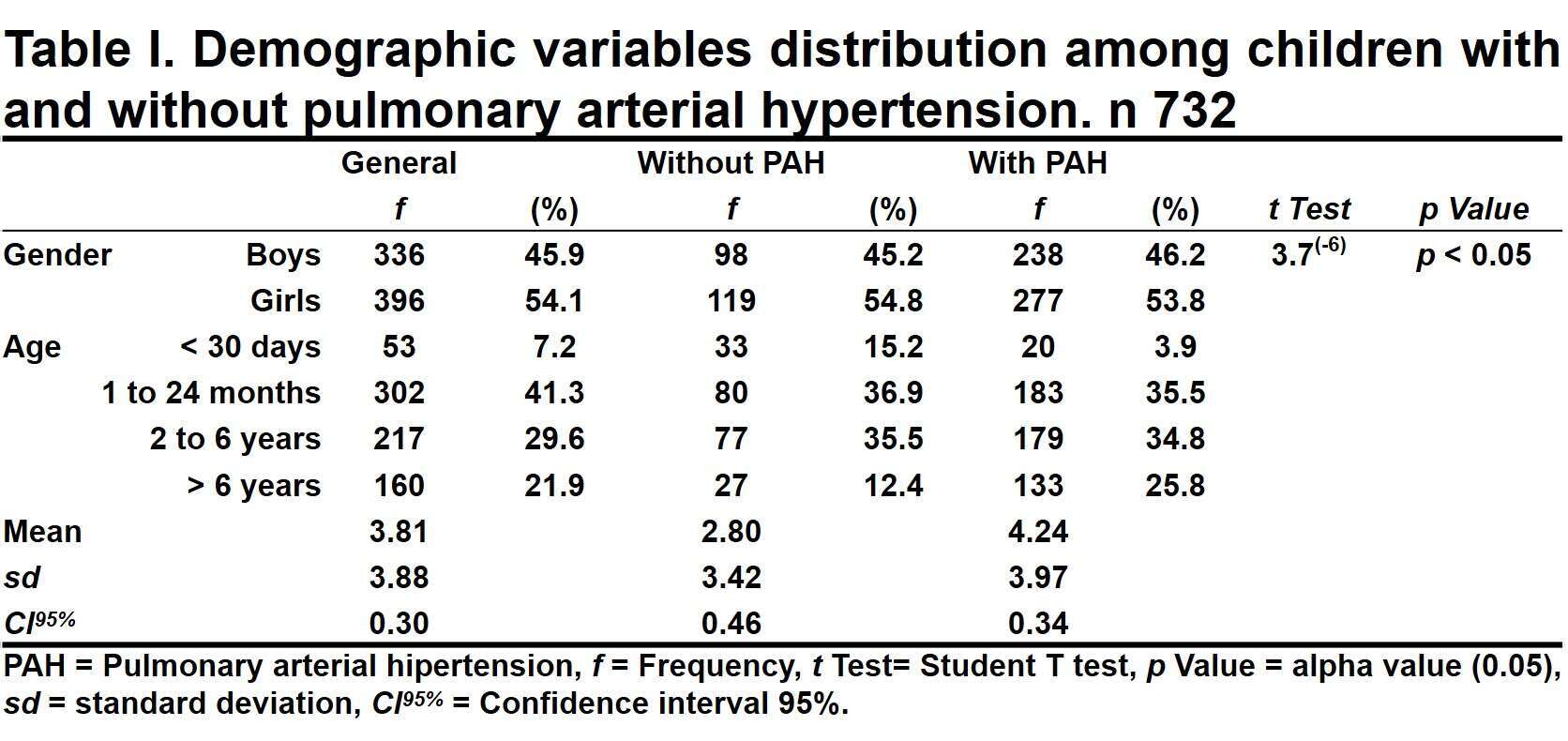
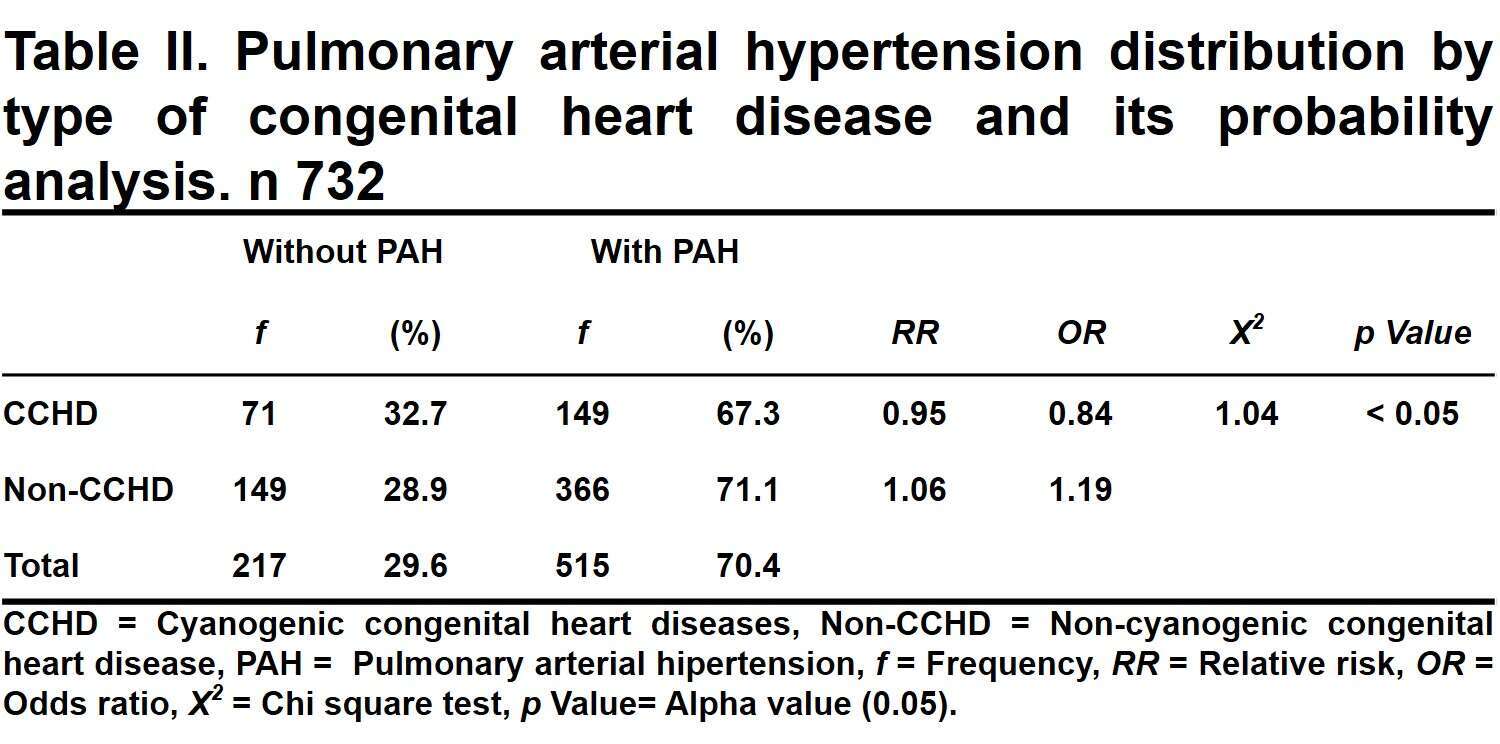
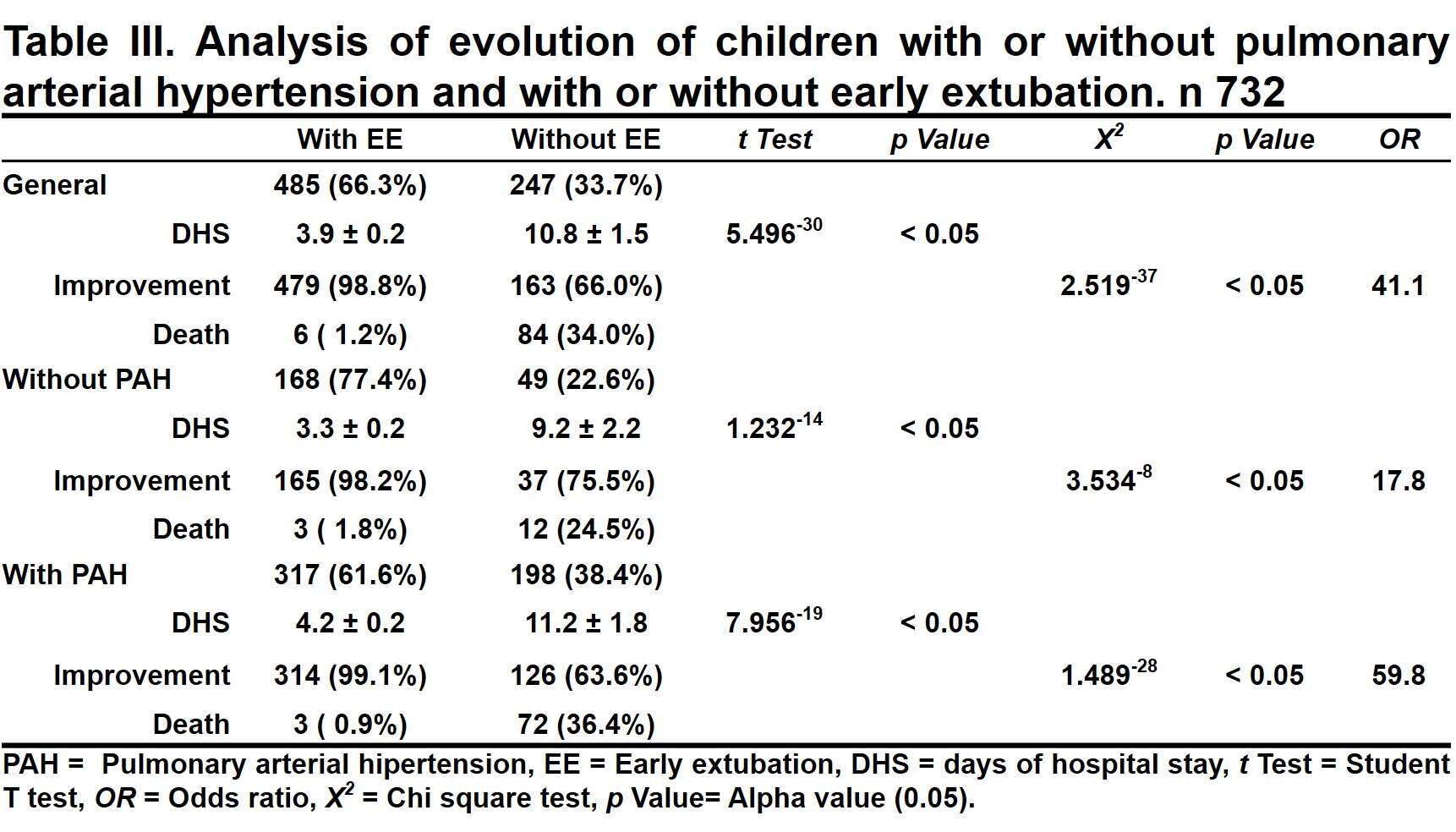
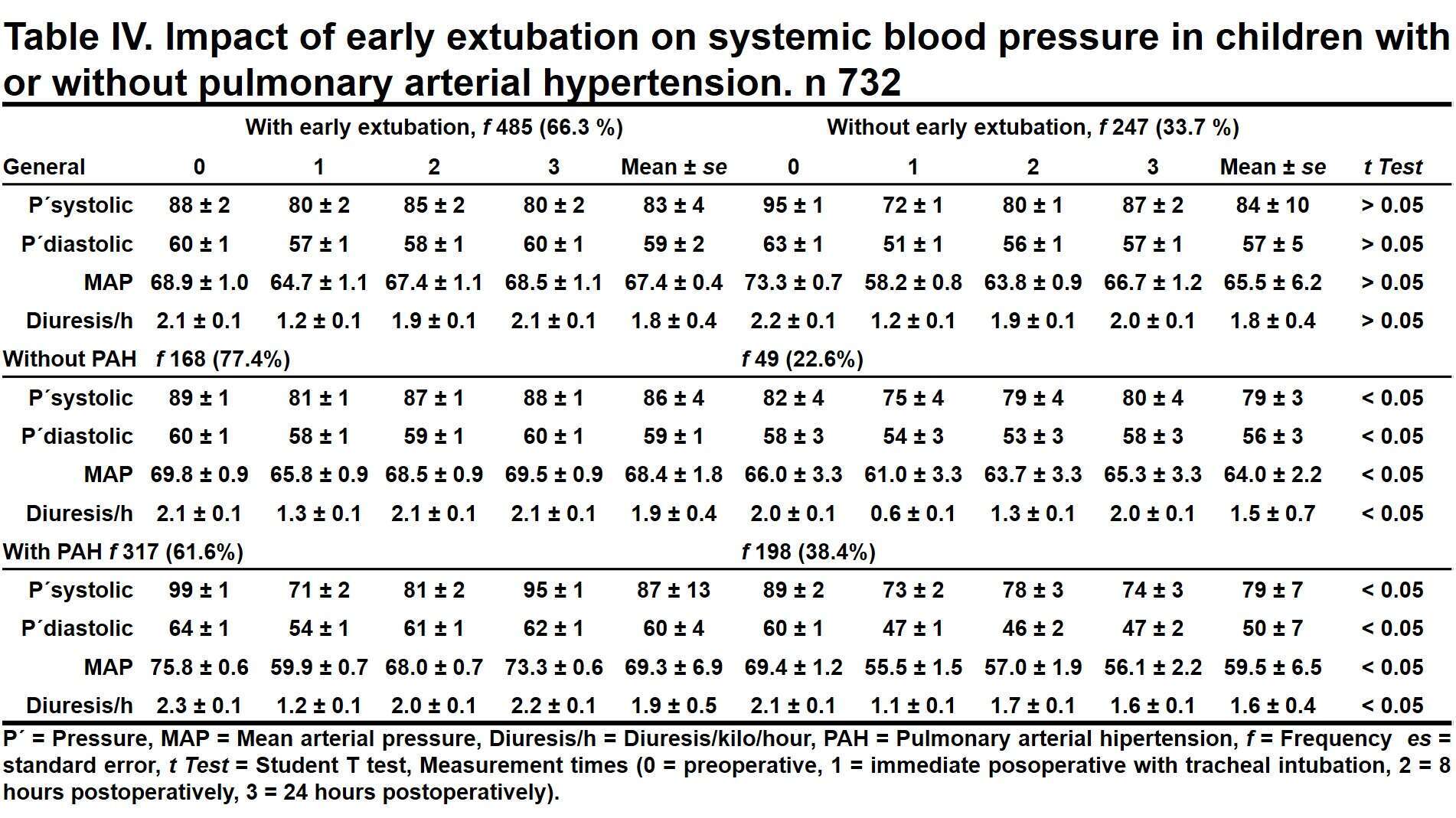
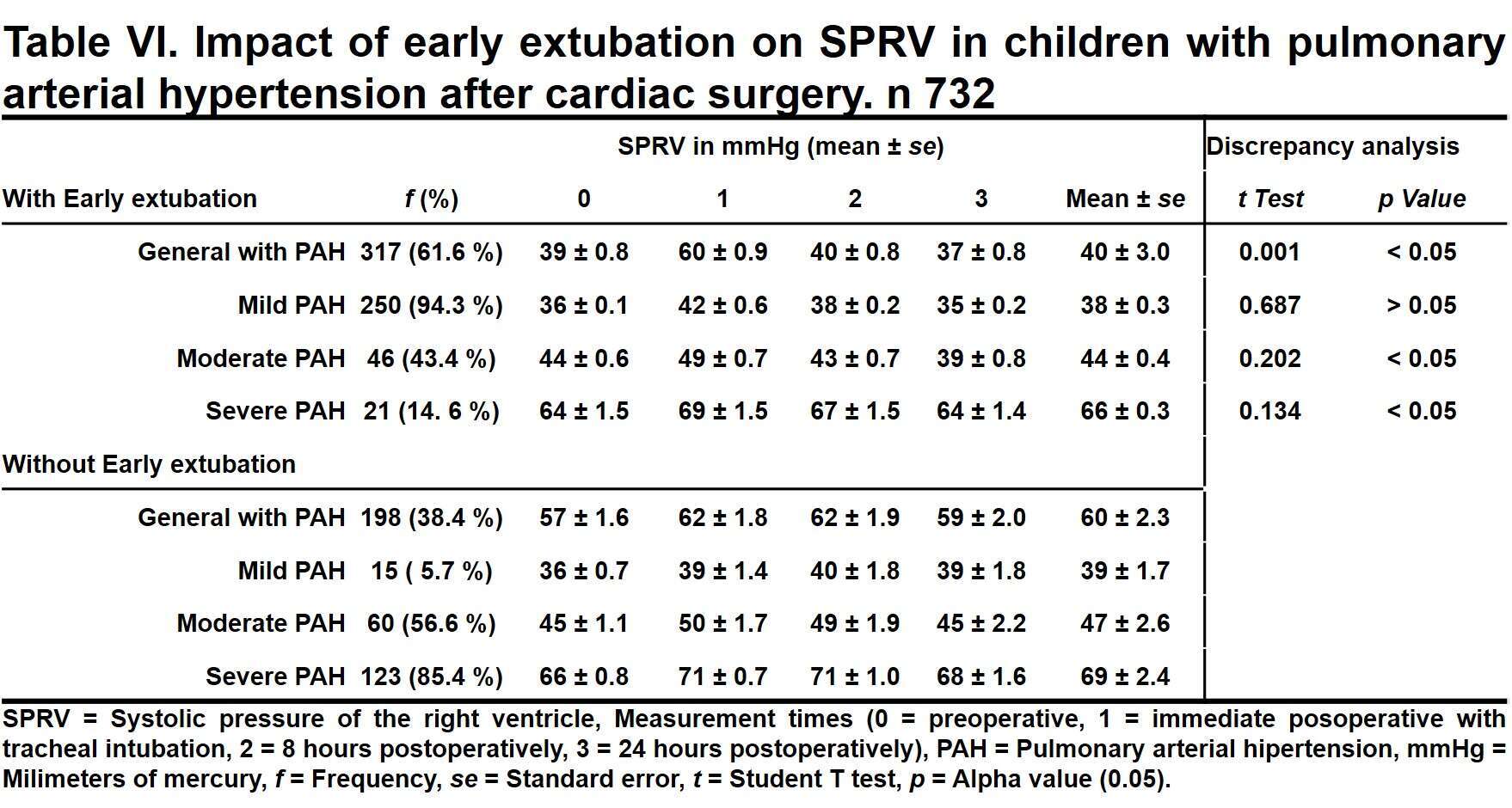
Methods: Data of 732 children 15 and younger undergoing cardiothoracic surgery between January 1, 2009 and December 31, 2018, were examined and distributed in groups with or without preoperative pulmonary arterial hypertension. Demographic variables, type of congenital heart disease, and clinical outcome were analyzed and compared between both groups. The hemodynamic impact of early extubation in both groups was evaluated by measuring blood pressure and hourly uresis in the preoperative period, immediately postoperative, 8 hours and 24 hours after cardiac surgery; pulmonary arterial pressure was assessed by measuring echocardiography of right ventricular systolic pressure at those same times.
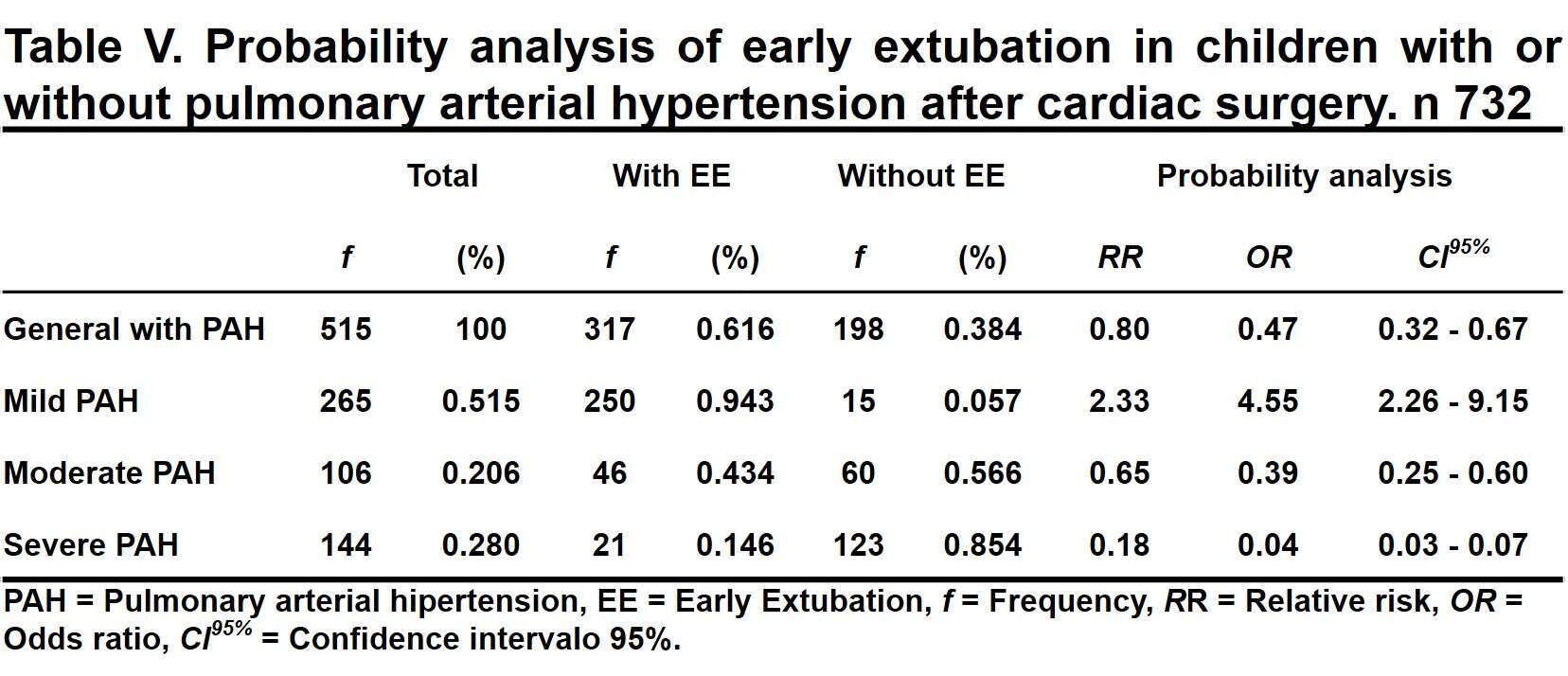
Results: In this study, 732 children (mean age 3.8 ± 0.3 years) underwent cardiac operations for various types of congenital heart disease. Of those children, 515 (70.4%) had pulmonary hypertension and 217 (29.6%) did not. Early extubation was performed in 485 (66.3%) patients and 98.8% successful. Without early extubation, the probability of death increased and became 58.9 times more likely in children with pulmonary hypertension. Early extubation was associated with improved mean arterial blood pressure and hourly uresis; and a reduction of pulmonary arterial pressure, even in cases of severe hypertension.
Conclustion: The pro-physiological effects of early extubation after pediatric cardiac surgery are associated with the good hemodynamic impact even in the presence of pulmonary arterial hypertension.
Powered by Eventact EMS