
Effect of High-Resolution Computed Tomograhy (HRCT) Results in Prognostic Evaluation of Bronchopulmonary Dysplasia (BPD) Cases
2Department of Pediatrics, The Kyrenia University, Dr Suat Günsel Hospital, Cyprus
3Department of Radiology, Akdeniz University, Turkey
4Department of Biostatistics and Medical Informatics, Akdeniz University, Turkey
5Department of Pediatrics, Division of Neonatology, School of Medicine, Akdeniz University, Turkey
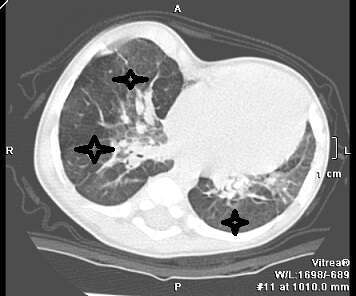
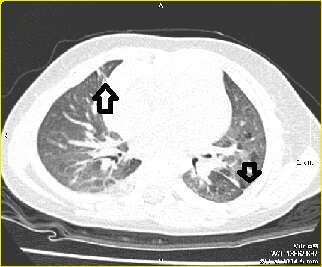
Objectives: BPD carries a risk of long term pulmonary sequale with changes in pulmonary mechanics and parenchyma. HRCT is a method of detecting such structural changes. Our aim was to characterize these structural abnormalities associated with BPD and to evaluate whether the severity of HRCT changes was associated with clinical findings.
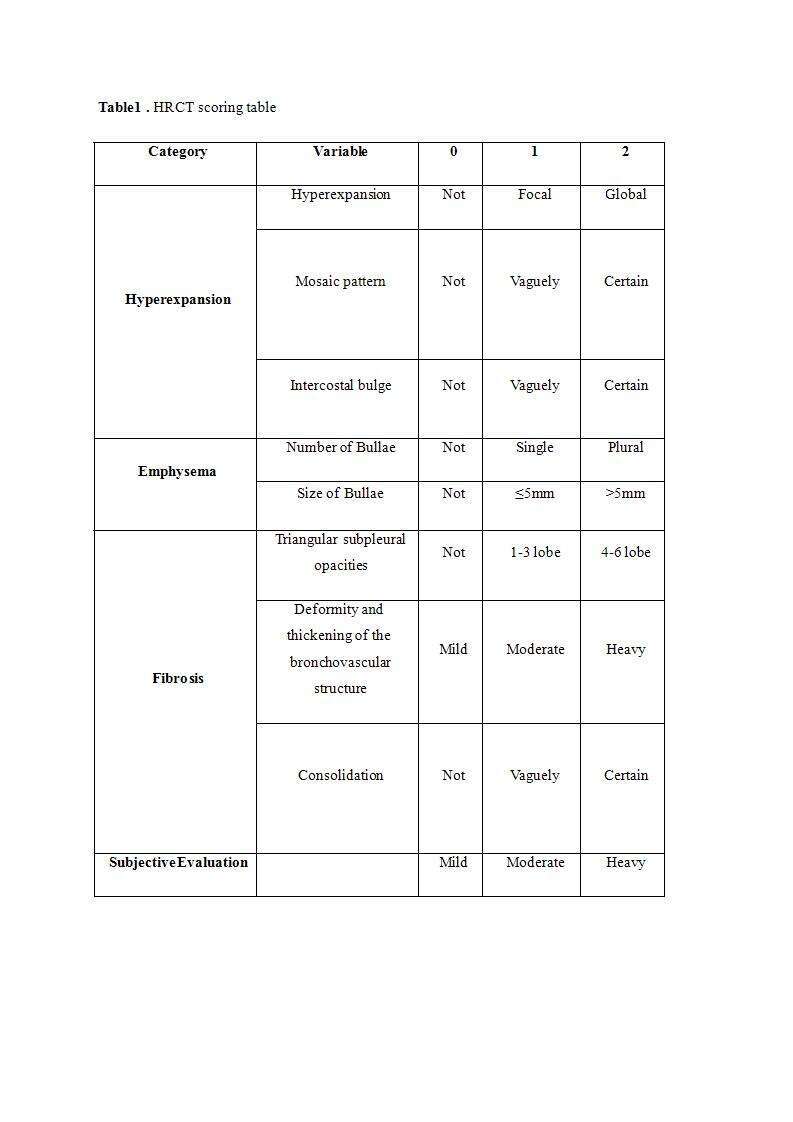
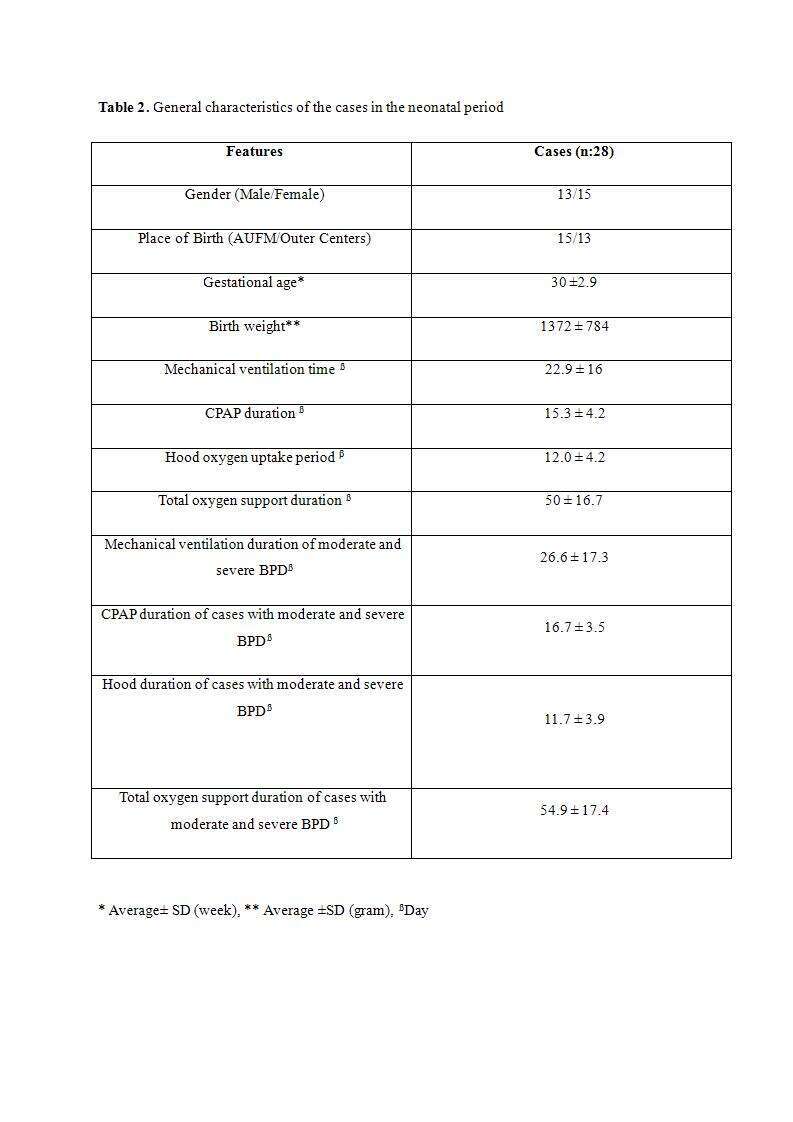
Methods: 28 patients born with a mean gestation age of 30 ± 2.9 weeks and diagnosed as BPD in their neonatal period were reevaluated when they were between the post natal ages of 6-12 months. They were divided into three groups as mild (n:8), moderate (n: 10), and severe (n: 10) according to their clinical data. HRCT scans were performed in patients with a history of moderate and severe BPD. One radiologist analysed scans using a structured scoring system.
Results: Their ages were between 9.8 ± 2.3 months at time of reevaluation.The average HRCT total score of patients was respectively moderate 7.20 ± 4.05 ; 7.40 ± 2.84 with severe BPD.The differerence between them was not significant (p = 0.620).Data obtained during the neonatal period, there was no significant correlation between the duration of oxygenation, the duration of mechanical ventilation, birth weights and the total HRCT scores performed at the time of reevaluation, in patients with moderate and severe BPD (p = 0.408, r = 0.183 for birth weights).
Conclusions: Those data suggest that the pathology detected in radiological imaging may not always be parallel to clinical findings and that the clinical course of infants with severe radiological data may be better or worse than expected. However, we believe more studies with larger number of patients and with different scoring systems are necessary in order to evaluate the role of HRCT in the clinical evaluation and long term prognosis of BPD.
Powered by Eventact EMS